- Al Sukhun S, Temin S, Barrios CH, Antone NZ, Guerra YC, Chavez-MacGregor M, Chopra R, Danso MA, Gomez HL, Homian NM, Kandil A, Kithaka B, Koczwara B, Moy B, Nakigudde G, Petracci FE, Rugo HS, El Saghir NS, Arun BK. Systemic Treatment of Patients With Metastatic Breast Cancer: ASCO Resource-Stratified Guideline. JCO Glob Oncol. 2024 Jan;10:e2300285. doi: 10.1200/GO.23.00285. PMID: 38206277; PMCID: PMC10793992.
ASCO guidelines on metastatic breast cancer announced
The new American Society of Clinical Oncology guidelines are a comprehensive tool addressing the divergent resources available to physicians.
Impact on patients worldwide
The authors of the recent guidelines on the systemic treatment of patients with metastatic breast cancer emphasise that the ultimate goal is to improve outcomes for breast cancer patients worldwide. The guidelines serve as a support system for physicians, allowing them to optimise care, lobby for resource allocation, and guide policy makers. It is their hope that these guidelines will contribute to better outcomes and quality of life for patients globally, particularly in resource-limited settings.
A four-level approach
The focus is on the care and treatment of metastatic breast cancer, considering the variable availability of resources globally. Considering breast cancer as the most common form of cancer worldwide, this guideline aims to consider different scenarios, such as those with abundant health resources and those with limited resources. In addition, the guidelines also consider other factors, e.g. the average age of affected patients in less fortunate regions, which is significantly lower - presenting additional challenges.
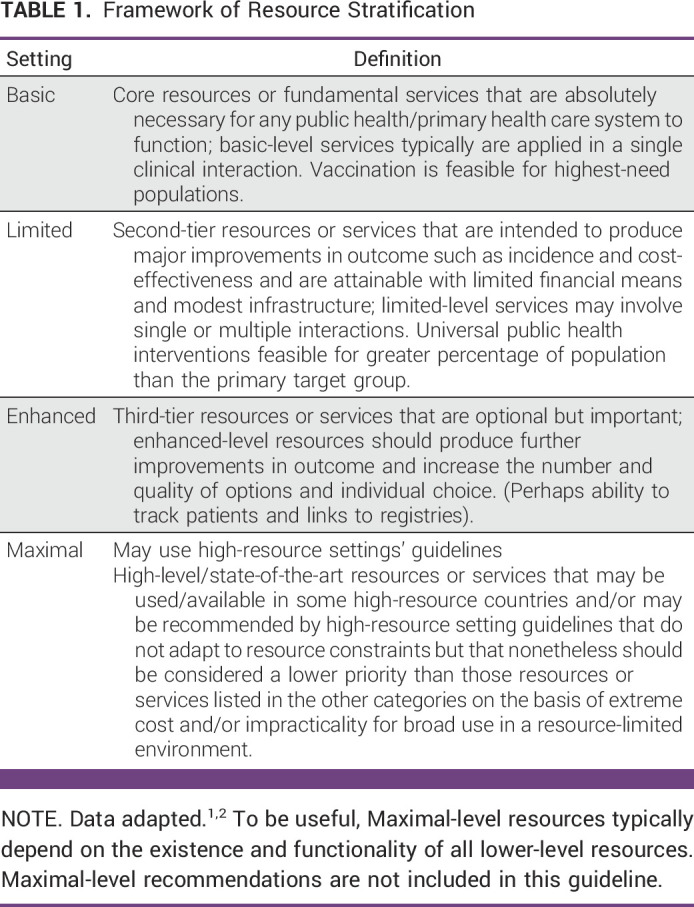
The four-level resource approach used in the development of the guidelines ranges from basic to maximal level, considering between the two extremes: a limited and an advanced context (in ascending order of resources we have, therefore, 1. basic context, 2. limited context, 3. advanced context, 4. maximal context). This framework recognises the variations not only between but also within countries. Below we provide the table as indicated in the guidelines.
The guidelines, taking into account available resources, support physicians in resource allocation and treatment decisions. For example, without a receptor assessment tools in basic settings, the guidelines advise physicians to assume hormone receptor positivity and initiate treatment with tamoxifen. This approach aims to provide a practical solution in resource-limited settings.
General notes
- Palliative care needs must be addressed for all patients at the time of presentation of MBC (Metastatic Breast Cancer), including situations where antineoplastic interventions are not accessible.
- Premenopausal patients may only take aromatase inhibitors if concomitant with ovarian ablation or ovarian suppression.
- Physicians should recommend therapy based on pathological features and biomarkers, when quality results are available (as defined by guidelines).
- Cases should be discussed using a multidisciplinary approach with the core team including surgeon, pathologist, oncologist and radiotherapist.
First-line therapy
HR+ breast cancer
- Assessment of menopausal status is crucial. Premenopausal patients should be recommended ovarian suppression or ablation. Patients whose tumours express any level of hormone receptors should be offered hormone therapy. In basic settings, if immunohistochemical examination is not available, physicians may assume hormone receptor positivity and administer tamoxifen in most cases.
- For patients with HR+ HER2- MBC, when non-steroidal aromatase inhibitors and CDK4/6 inhibitors are missing, hormone therapy alone should be used. For severe disease, physicians may use single agent chemotherapy; surgery may be used in cases requiring 'salvage mastectomies' and for local control.
- For patients with MBC HR+ HER2- in premenopause, ovarian suppression or ablation plus hormone therapy should be proposed.
- Patients with HR+ HER2- MBC who are offered chemotherapy should be offered single agent chemotherapy rather than chemotherapy with combination agents, although combination regimens may be proposed for highly symptomatic or life-threatening disease.
- HR+ MBC patients with disease progression who are being treated with an endocrine agent and who are post-menopausal may be proposed:
- endocrine therapy with or without targeted therapy or
- single-agent chemotherapy.
- Patients with premenopausal HR+ MBC without previous hormonal therapy may be treated with:
- tamoxifen, ovarian ablation or ovarian suppression alone, or subsequent hormone therapy, or non-steroidal aromatase inhibitors with ovarian ablation or ovarian suppression and CDK4/6 inhibitors in advanced settings;
- tamoxifen, or ovarian ablation or ovarian suppression with hormone therapy in limited settings;
- tamoxifen in basic settings.
- HR+ MBC patients with disease progression with an endocrine agent and premenopausal may be offered treatment with:
- ovarian ablation or ovarian suppression with hormone therapy or subsequent hormone therapy in advanced settings;
- alternative hormone therapy or surgery in limited contexts;
- tamoxifen and bilateral oophorectomy in basic settings.
HER2+ breast cancer
- HER2-targeted therapy is recommended for patients with HER2+ advanced breast cancer, with the exception of those with clinical congestive heart failure or significantly impaired left ventricular ejection fraction, which should be evaluated on a case-by-case basis.
- Trastuzumab, pertuzumab and taxanes are recommended for first-line treatment. If pertuzumab is not available, physicians may administer chemotherapy and trastuzumab in advanced settings. In limited settings, chemotherapy alone may be proposed.
- For patients with HER2+ and HR+ MBC, HER2-targeted therapies and chemotherapy or endocrine therapy alone may be proposed, or chemotherapy or endocrine therapy alone, depending on the availability of anti-HER2 therapies.
Triple-negative breast cancer
- Patients with triple negative and known PD-L1+ MBC may be offered the addition of an immune checkpoint inhibitor to chemotherapy as first-line therapy in advanced settings. In limited settings, most patients with triple-negative MBC may be offered chemotherapy alone.
- Patients with triple negative MBC and PD-L1- should be given single agent chemotherapy rather than combination chemotherapy as first-line treatment.
- In advanced settings, BRCA1 or BRCA2 mutation carriers with HR- HER2- metastatic breast cancer may be offered PARPi therapy.
- Patients with HR+ MBC and known BRCA mutations, if PARPi therapy is not available, may be treated with hormone therapy with or without ovarian ablation.
Second line
HR+ breast cancer
In advanced settings, recommendations depend on prior therapy. For example, in cases of previous endocrine therapy, physicians may offer second-line endocrine therapy with or without targeted therapy (e.g. CDK4/6 inhibitor or everolimus). In limited settings with prior endocrine therapy, physicians may propose second-line endocrine therapy if available, otherwise they may propose chemotherapy.
HER2+ breast cancer
HER2-targeted therapy should be administered according to prior therapy and hormone receptor status. Trastuzumab deruxtecan or alternative HER2-targeted therapy regimens may be offered as second-line treatment depending on availability. In limited settings, chemotherapy (with trastuzumab, if available) may be offered. In basic settings, if a patient has had previous treatment and nothing else is available, if she presents with symptoms, physicians may propose primary surgery for palliative reasons, including local control. If a patient has completed adjuvant trastuzumab treatment less than a year before relapse, second-line options may be offered. If more than one year has elapsed, offer first-line options.
HER2+ breast cancer with BRCA1/2 mutations
HR+ MBC patients with BRCA1/2 mutations who no longer benefit from endocrine therapy may be offered PARPi therapy rather than chemotherapy.
Triple negative breast cancer
- As a second-line treatment, with or without prior PD-L1 checkpoint inhibitors, physicians may offer chemotherapy if sacituzumab govitecan not be available.
- Patients with triple-negative MBC with germline BRCA1/2 mutations previously treated with chemotherapy may be offered treatment with PARPi rather than chemotherapy.
Third line
HER2+ breast cancer
In the third line, physicians should propose other combinations of HER2-targeted therapies. For patients with HER2+ and HR+ MBC, offer hormone therapy with or without trastuzumab.
Triple negative breast cancer
In third line, patients with triple negative MBC may be eligible for PARPi (if BRCA1/2 germline mutation status is known). If not available, physicians may offer chemotherapy and/or palliative care.
Conclusions
The authors point out the insufficiency of research on cancer therapy conducted in resource-limited settings. They consider it important to further research on metastatic breast cancer in resource-limited settings, considering the issues of access to surgery and chemotherapy, treatment efficacy and cost-effectiveness.
They also point out that although guidelines are crucial, personalised care for the patient, considering social, physical and tumour-related aspects, is essential.