- Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022 Sep 14;378:e070442. doi: 10.1136/bmj-2022-070442.
- ”Going through the motions": A qualitative exploration of the impact of emergency medicine resident burnout on patient care. AEM Educ Train. 2022 Sep 27;6(5):e10809. doi: 10.1002/aet2.10809.
Burnout in the ER: when the tank is empty, everyone suffers
Burnout hits emergency service teams in particular. The results of a large-scale study are clear: when caregivers suffer, patient safety is at stake.
Translated from the original French version.
About the author:
Nicolas Peschanski is a professor of emergency medicine and a hospital practitioner at the Rennes University Hospital (France). Prof. Peschanski's international career, particularly in the USA, has enabled him to become a member of the International Commission of the American College of Emergency Physicians as well as the steering committee of the EMCREG-International (Emergency Medicine Cardiac Research and Education Group). He is also a member of the European Society for Emergency Medicine (Eusem) and more particularly of its "Web & social media" committee. Prof. Peschanski is a strong supporter of the FOAMed principle (Free Open Access Meducation). He uses social networks (@DocNikko) for educational purposes and to share knowledge about the emergency medicine field.
The state of burnout
Health systems around the world are facing a serious workforce crisis. An increasing number of physicians are working part-time, resigning or taking early retirement in response to excessive workloads and symptoms of burnout. These are mainly frontline physicians in emergency medicine and intensive care.
Physician burnout has considerable deleterious effects, firstly on themselves, but also on hospital departments and the entire healthcare system. The quality of care, safety and patient satisfaction are compromised.
The article1 presented here is the result of the largest study ever conducted on this subject: a systematic review of all the literature and a meta-analysis of 170 observational studies - 48 of them European - on burnout symptoms. In the end, the data obtained concerned 239,246 physicians.
What did the authors of this study discover? And above all: what can we learn from it in order to change our practice in emergency medicine?
Impact on caregivers and patients
Regarding the primary endpoint, the conclusion of the authors of this study is clear: yes, burnout harms both caregivers (medical and paramedical) and patients.
The researchers found significant associations with burnout, namely:
- Job dissatisfaction
- Regret about career choice
- Frequent desire to change jobs
- Hindrance to career development
- Reduced productivity
Concerning the quality of care:
- A decrease in professional rigour and professionalism in particular
- An increase in incidents and undesirable events
- Decrease in patient satisfaction
This remarkable work also provides us with evidence on the profile of physicians most likely to be affected (however, these associations no longer appear in a multivariate regression analysis).
According to this study, victims of burnout are more frequently:
- Hospital physicians
- Physicians between 31 and 50 years old
- Emergency physicians, resuscitators and intensivists
From burnout to a decline in the quality of care
Until now, no meta-analysis had examined the association between physicians' burnout and their professional commitment, and therefore the quality of care.
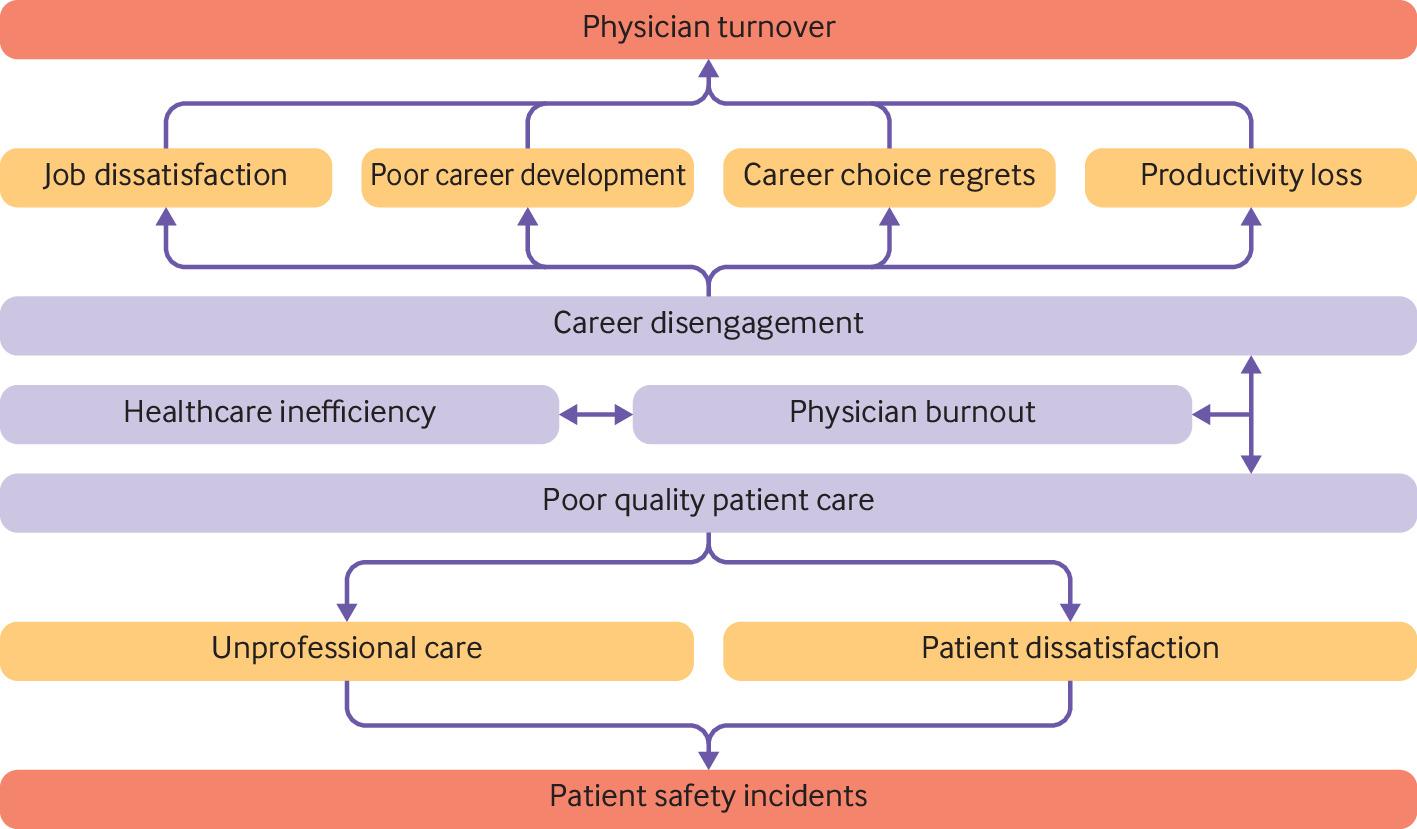
Diagram from the article: "Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis" representing the flow of associations between physician burnout, career engagement, and quality of care. The outcomes assessed in the analysis are highlighted in yellow or red. Those in red show a potential increased risk compared to those in yellow.
For the authors, this study provides "compelling evidence that physician burnout is strongly associated with physician disengagement and suboptimal patient care." They explain that physicians experiencing burnout are:
- Twice as likely to be involved in patient safety incidents.These incidents are more common among younger physicians working in emergency medicine and intensive care.
- More than twice as likely to receive low patient satisfaction ratings.
- More than three times more likely to intend to leave their job (turnover) or regret their career choice.
If they feel that they are short of time, these physicians may end up taking more unnecessary risks. The occurrence of an adverse event - or simply the realisation that the quality of care provided is poor - can then lead to burnout. The authors refer to this process as "secondary trauma".
Different effects depending on the components of burnout
Burnout is classically defined as a syndrome involving three dimensions:
- Emotional exhaustion: feeling constantly overwhelmed, unable to cope.
- Depersonalisation or cynicism: in the health professions, this component manifests itself in a loss of empathy, excessive detachment, etc.
- Reduced efficiency, with a decreased sense of competence.
This study shows the following links:
- Physicians with high emotional exhaustion scores are particularly likely to express intentions to leave their jobs.
- Those with high depersonalisation scores are particularly likely to be involved in poorer quality care.
For the authors, interventions with the physicians concerned should therefore be proposed in subgroups, depending on which dimension of burnout is predominant.
Why are these results important for us emergency physicians?
Firstly, when we see that patient safety is particularly affected by young, burnt out physicians, especially among emergency physicians, I find the association striking. When we explore the mysteries of this meta-analysis, we also learn that professional dissatisfaction is strongly associated with the fact of being an intern; all the more so if it is a hospital specialty, and especially within an emergency department.
Moreover, burnout is not only harmful to physicians, and not only psychologically. It has a negative impact on safety, quality of care and patient satisfaction. In this study, the authors also mention the huge economic consequences of lost efficiency and adverse events.
To reduce the risk of burnout, it is not enough to bring croissants on Sunday mornings (but let's keep that "tradition"!). Let's make sure that the workload in our departments remains reasonable. Let's continuously develop a culture of healthy professional interactions, whether with each other, with our peers in other specialties, or with our administrations.
Finally, within emergency medicine, we must ensure that each individual is recognised and can develop throughout their career. Let's pay special attention to our interns, and then to physicians at the beginning of their careers.2
Interns and emergency physicians are particularly vulnerable to burnout, which is more dangerous for patients than elsewhere... These are two good reasons to be extra vigilant in our departments and among our troops.
Professor Peschanski declares the following relations of interest:
- Over the last three years: Vygon SA (consultant), Fisher&Paykel (symposium), AstraZeneca (symposium).
- Over the last twenty years (Symposia): Fisher&Paykel Healthcare , AstraZeneca, Lilly, Sanofi, Daiichi-Sankyo, HeartScape, The Medicine Company, Thermofisher, Roche Diagnostics.
- Over the last twenty years (Boards): Bayer, AstraZeneca, Vygon SA, Portola USA, Sanofi, Boehringer Ingelheim.
- Over the last twenty years (Congresses): Lilly, Sanofi, Vygon SA, Portola, Roche Diagnostics, Thermofisher.
- Over the last twenty years (Research funds, non-personal): Servier, Boehringer Ingelheim