- Kinj R. et al. (2022). Stereotactic Body Radiation Therapy in Patients with Oligometastatic Disease: Clinical State of the Art and Perspectives. Cancers (Basel). 2022 Feb 23;14(5):1152.
- Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
PMC Copyright notice
Effective oligometastases treatment: stereotactic radio-therapy hits 90% control rate
SBRT can be used for different categories of oligometastatic disease. The disease covers a broad spectrum. A summary of its manifestations and treatment.
What exactly is stereotactic radiotherapy?
Stereotactic radiotherapy (SBRT) is a type of radiotherapy in which a small number of high-dose radiation beams are delivered to a target volume using highly precise equipment in order to maximise cancer control while minimising side effects on healthy tissue. The exact role of SBRT varies depending on the primary location and subtype of the oligometastatic condition. In this image-guided radiotherapy technique, small target volumes are irradiated with high precision and high doses in a single fraction or a few fractions. The advantage of this method is that it significantly minimises radiation exposure to surrounding tissue.1
The role of SBRT in oncology is being thoroughly investigated
SBRT is of crucial importance in two stages of cancer:
- in the early stage of the primary tumour
- in oligometastatic disease
In these stages of cancer, SBRT is used with the aim of achieving complete remission of the tumour. Over the years, a growing body of clinical evidence has accumulated for the use of this treatment method. This review evaluates the role of SBRT in the treatment of oligometastases. This analysis primarily examined the technical and clinical aspects of SBRT depending on the type of disease and clinical indication. A total of 972 publications were identified, of which 66 were evaluated.1
What is special about oligometastatic disease?
Oligometastatic disease is a stage of the disease that can still be treated curatively. Oligometastatic disease lies between locally advanced and metastatic disease. It can be divided into four categories:
- De novo oligometastases: newly diagnosed tumour disease with only a few metastases.
- Oligo-recidivism: recurrence in a few new metastatic sites in patients who have already been treated for metastatic disease.
- Oligo-progression: disease progression in a few metastatic sites in patients whose cancer could otherwise be controlled by systemic treatment,
- Oligo-persistence: despite responding to systemic treatment, a few metastatic sites are still present in the affected patients.
These four categories correspond to the various clinical scenarios that can occur in oligometastatic disease and thus cover the spectrum of the disease. Depending on their response to systemic treatment, affected patients may progress through the different categories of oligometastatic disease.1
Treatment options for oligometastatic disease
Ablative treatments for oligometastases include SBRT, local surgery and radioablation. These therapeutic options must be as curative as possible in order to effectively control oligometastatic disease.1
Steps for planning stereotactic body radiotherapy
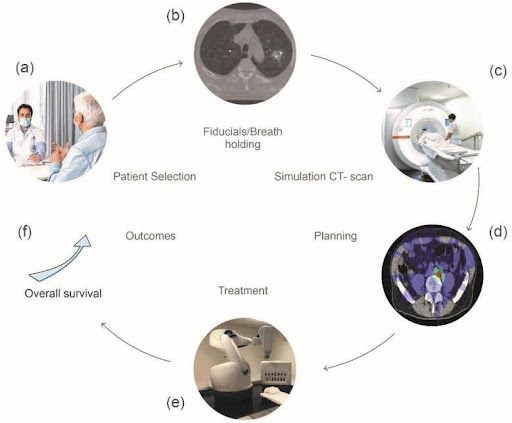
Figure 1: (a) Consultation with the patient to discuss treatment goals and possible side effects. (b) Placement of markers for tumour tracking throughout treatment. (c) 3D imaging using CT scan for precise tumour localisation. (d) Dosimetry planning to determine the radiation dose and positioning of the beams. (e) Performing treatment with state-of-the-art equipment that enables daily imaging to ensure correct positioning of the tumour. (f) Some studies have observed a possible prolongation of overall survival.2
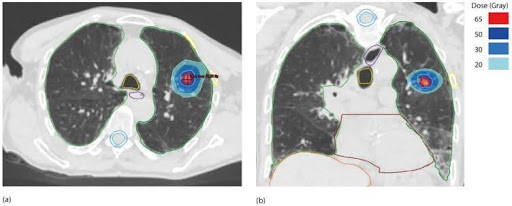
Figure 2: This figure shows an example of the application of SBRT in metastatic lung cancer: dosimetry of a 55 Gy lung SBRT in five fractions of 11 Gy each for lung metastases of primary lung cancer. (a) Axial view, (b) coronal view. The gross tumour volume (GTV) is shown in red, the planning target volume (PTV) in blue and the marker points in green.2
Proof-of-concept results from the randomised SABR-COMET study as the basis for SBRT
In order to improve the precision of treatment despite organ movement, the adaptive technology of SBRT is constantly being further developed, resulting in fewer and fewer side effects. To date, findings on the treatment of oligometastases are based on the proof-of-concept results of the randomised SABR-COMET study. These results demonstrated a significant prolongation of overall survival with SBRT compared to the best supportive care. Future studies should consider the following factors:
- Randomisation of patients according to disease type and location
- Long-term follow-up of treated patients
Conclusion for medical practice
- Stereotactic body radiation therapy (SBRT) scores highly thanks to its excellent tolerability and high locoregional control rates of up to 90%.
- The findings on the treatment of oligometastases using SBRT are based on the proof-of-concept results of the randomised SABR-COMET study.
- Oligometastatic diseases can be divided into four categories.
- Randomisation of patients according to disease type and location plays an important role in future studies.