Intensive care: (re)open to family members
An Italian team has published a paper on the benefits of allowing ICU visits during a pandemic period, proposing essential policy and operational options for implementation.
The proposal aims to restore good 'humanizing' practices in both intensive and non-intensive care units
Due to the COVID-19 pandemic, visits to patients by family members were prohibited. An Italian team has published a paper in the journal Critical Care on the benefits of allowing ICU visits during a pandemic period, proposing essential policy objectives and an operational guide to achieve them.
At the beginning of the health crisis caused by the SARS-CoV-2 virus, it was decided to prohibite family members from visiting their loved ones in hospital. These rules, which are mostly still in force, are often considered unfair by people who would like to be close to their loved ones, especially during the critical phases of an illness.
According to the paper authors, although the situation in COVID-19 wards remains extremely challenging, and while recognising the complexity involved in implementing protocols for the admission of family members, it is essential to find shared strategies adaptable to each local context to allow family members to enter COVID-19 wards.
Open intensive care: the benefits outweigh the risks
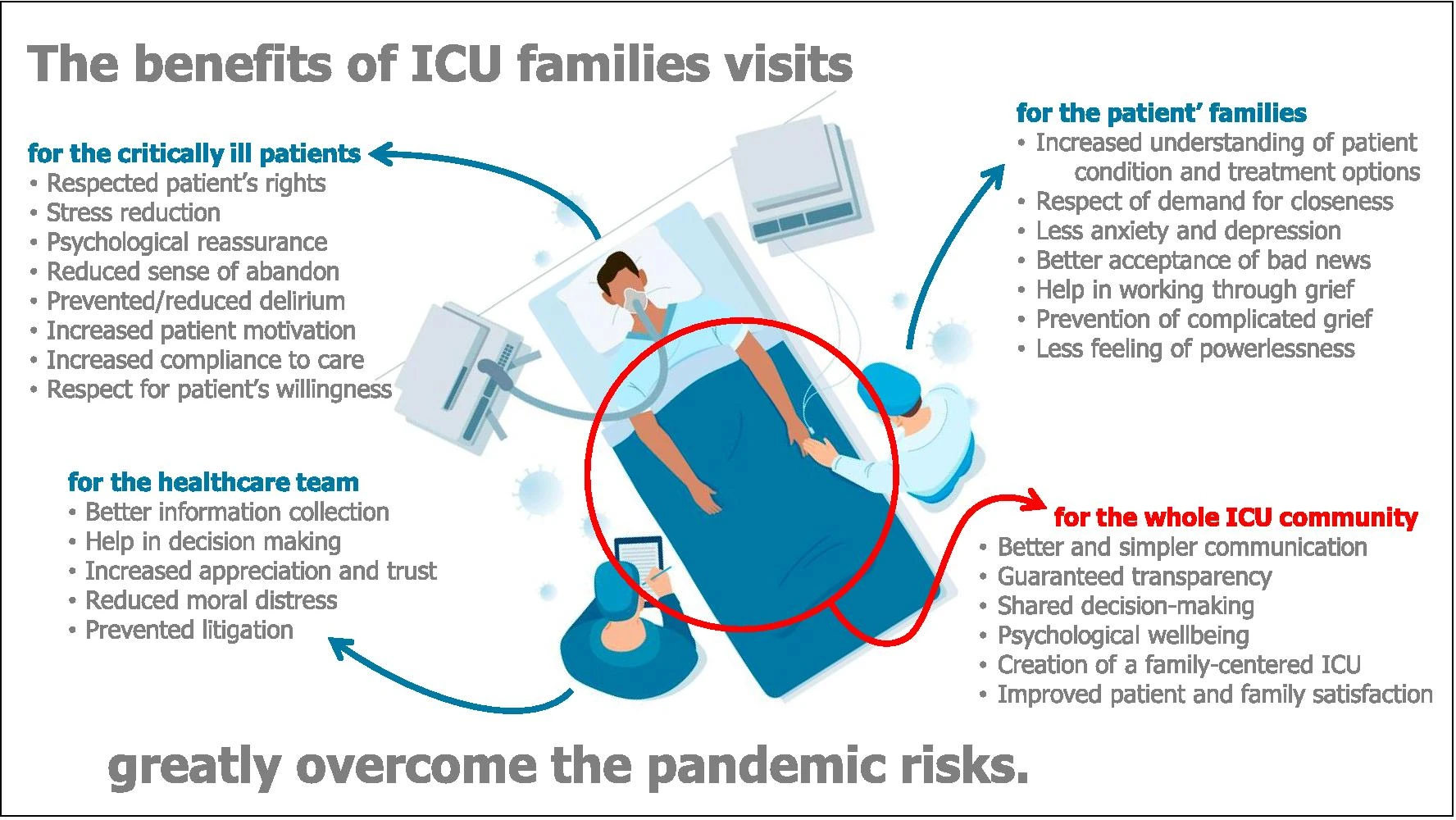
According to the authors, the benefits of having family members present in intensive care far outweigh the pandemic risks, which can be controlled by specific protocols. Phone and video calls are not enough. The physical presence of family members makes it easier to share care strategies. It allows more effective information, greater transparency and better understanding of decision-making processes, and makes it more feasible to share care choices.
From a clinical point of view, the presence of family members offers relational benefits, especially in certain phases (e.g. at the end of the deep sedation phase). The presence of family members also strongly motivates the patient to continue the necessary treatment. Even if limited in time and conditioned by the necessary PPE, visits respond to the patient's need, increases the trust of family members and the appreciation of the care team, and diminishes the understandable difficulty of family members in accepting bad news.
The possibility of being physically close to the loved one even at the time of death, if requested by the family, helps to reduce the risk of developing psychological traumas, which may persist for a long time.
Suggestions for opening the intensive care unit
- Family members should be admitted, even if only for short periods. Compared to no visits, even short visits often have substantial meaning for relatives and patients.
- Different rules should be established for COVID-19 and COVID-free ICUs - Simple protocols are needed. Relatives should be given clear, well-defined and unambiguous instructions, and their implementation should be carefully supervised.
- If the total number of family visits has to be limited, it is wise to facilitate visits for those who can benefit most. If the number of visits has to be limited, it is wise to favour visits that can offer the greatest possible benefit to the greatest number of both patients and visitors.
- It is advisable to set up a special ICU working group and to reassess (at least monthly) the structural and organisational conditions that justify limiting family visits.
- Relatives and other visitors should be informed about the risks of accessing COVID-19 areas.
- The reopening process should be shared with the whole team.
- The physical presence of relatives should not be limited to intensive care units - The decision to "open" should cover intensive care along with all other departments of the hospital, whose work always precedes or follows that of treating the most critical and complex phase of the illness.
How to proceed with ICU openings
The prerequisites for visitors to enter the hospital should be:
- The family member and the patient want it.
- The family member is not in fiduciary home isolation or quarantine.
- The family member is asymptomatic and has no risk factors for contagious diseases; sufficient PPE is available for family members.
- The presence of trained people (health workers or hospital volunteers) is guaranteed, with the task of indicating the internal routes, explaining in a clear and easily understandable way to non-experts how to use PPE correctly and supervising its correct use.
Next are the indications given in the published paper for proceeding with the opening of intensive care units:
- Use strict and agreed procedures to differentiate entry and exit routes, to ensure adequate scheduling, inter-personal distance, hand washing and mandatory wearing of PPE.
- Provide clinical monitoring of visitors (checking body temperature, absence of flu symptoms and other risk factors). Optional infectious surveillance with rapid antigen tests could give an answer within minutes and is not too expensive.
- Schedule visits so that people do not linger in waiting rooms and avoid too many relatives together at the same time. Limit the number of relatives/visitors per patient and - if it is not possible to arrange a daily visit - consider ensuring family visits at least once or twice a week.
- Allow exceptions in circumstances where it is particularly important to allow family members to visit the patient, such as during prolonged hospitalisation, in cases of poor short-term prognosis, and in all cases of particular patient frailty.
A hospital model closed to family members is not acceptable
The pandemic abruptly interrupted a decade-long process of 'humanisation' and 'openness' of intensive care units. According to the authors, current knowledge and the availability of personal protective equipment (PPE) make it possible to encourage a careful and gradual resumption of the opening to family visits, while fully respecting the patient's wishes.
The authors consider that there is no substantial reason why family members should not be admitted to COVID-19 wards. It may not only be useful, but even necessary. In the specific context of each hospital, they believe it is necessary to do everything possible to promptly re-establish good "humanizing" practices in both intensive and non-intensive care units.
Source:
Mistraletti, G., Giannini, A., Gristina, G. et al. Why and how to open intensive care units to family visits during the pandemic. Crit Care 25, 191 (2021). https://doi.org/10.1186/s13054-021-03608-3