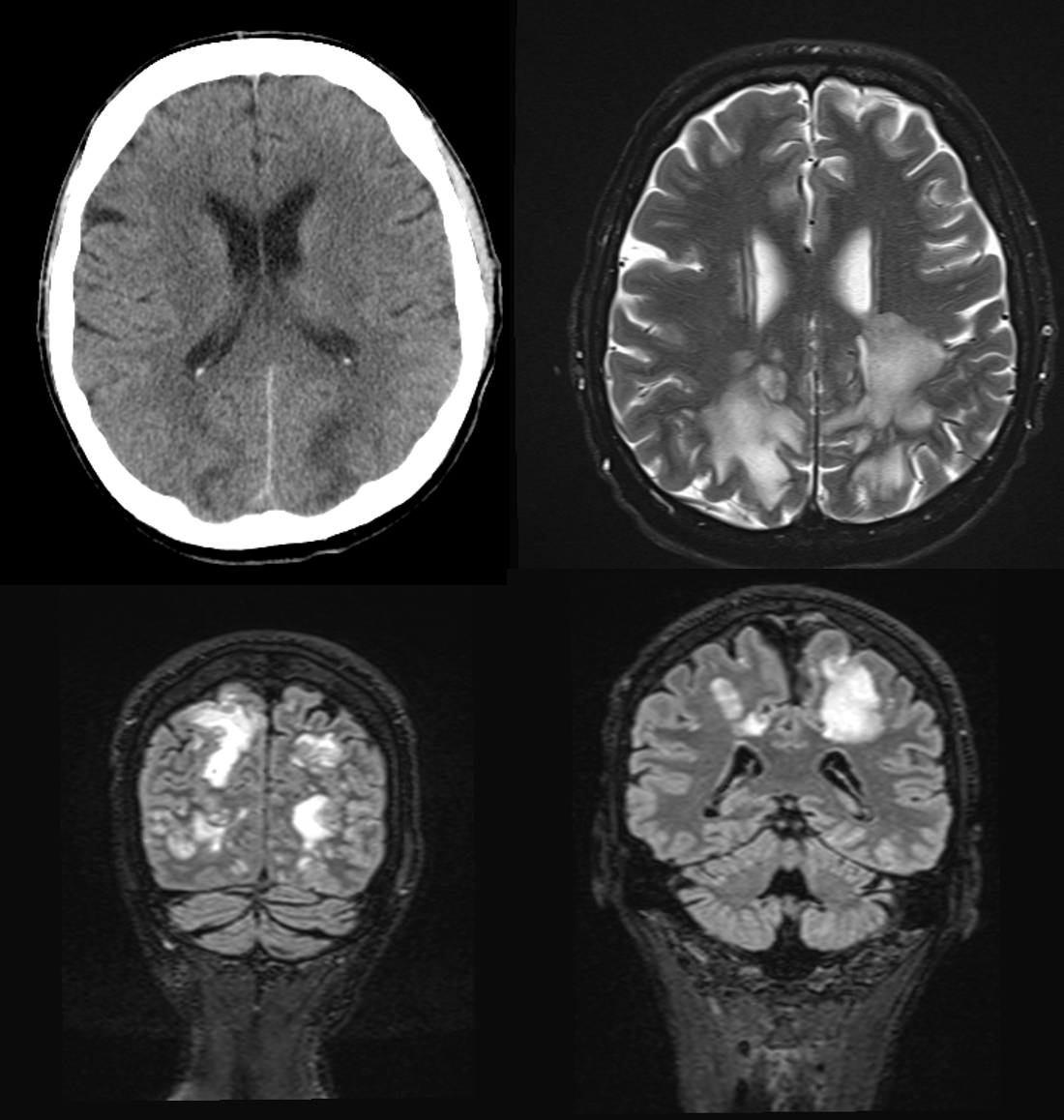
MRI findings
The axial T2 as well as the coronal T2-FLAIR sequences show pronounced flat T2w-hyperintense areas in the parieto-occipital semioval center on both sides. The cortex was not affected. Furthermore, there was no evidence of intracranial haemorrhage. Image was compatible with vasogenic oedema in posterior reversible encephalopathy syndrome (PRES).
Diagnosis and treatment
A PRES diagnosis was finally made. Posterior reversible encephalopathy syndrome is characterised by vasogenic oedema, often triggered by rapid fluctuations in blood pressure, renal insufficiency or the use of immunosuppressants. Mr F's long-standing hypertension, coupled with his recent deterioration in renal function, fitted this picture well.
Admission to the stroke unit focussed on immediate reduction of blood pressure and monitoring of his neurological function. Anticonvulsant therapy was initiated as a precautionary measure.
Clinical symptoms, treatment and prognosis of PRES
The clinical features of PRES are varied and can range from headaches and visual disturbances to nausea and altered mental status. Fortunately, the syndrome is often reversible, provided the underlying cause is treated effectively.
Mr F. responded well to the treatment. His blood pressure normalised within a few days and his neurological symptoms also improved. He was informed about the importance of controlling his blood pressure, and of regularly monitoring his kidney function. He was able to leave the hospital after a week, but with a strict treatment plan and regular follow-up appointments.