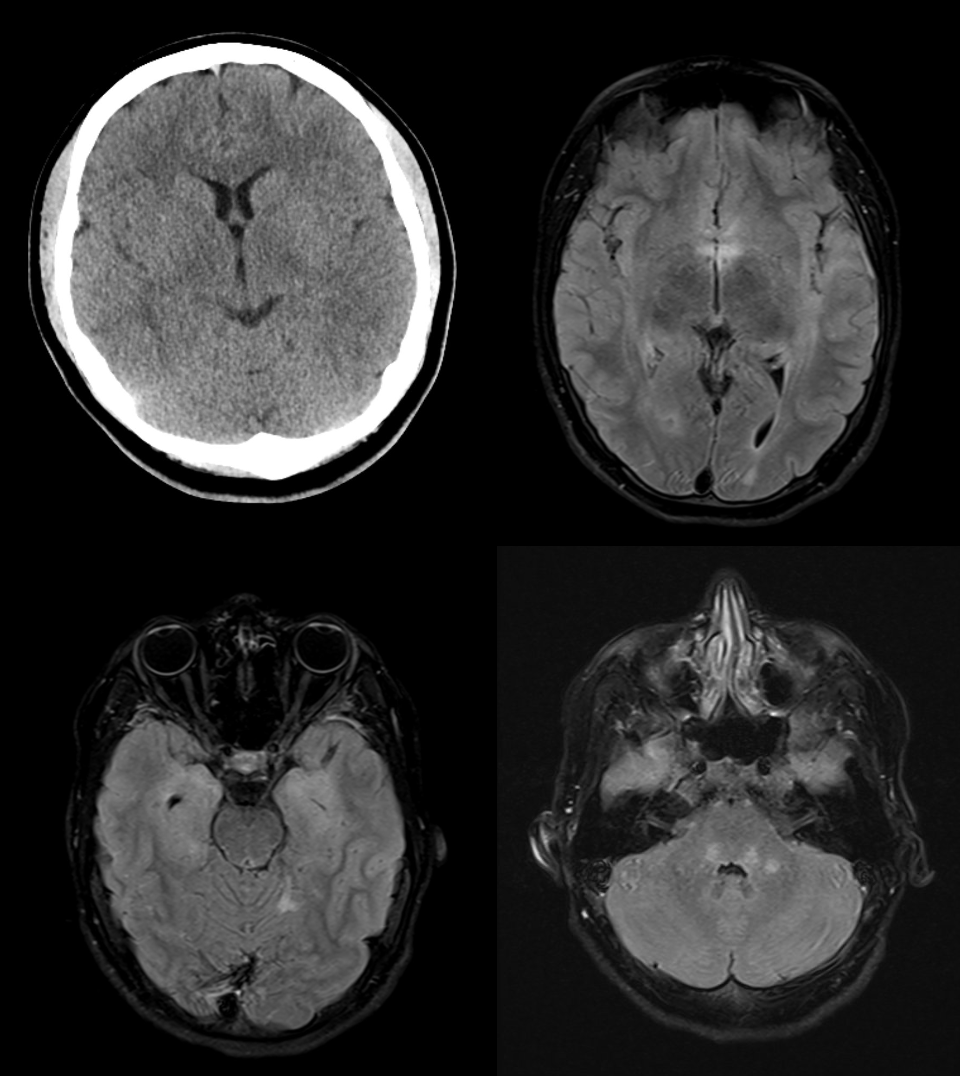
MRI findings:
MRI examination showed marked T2w hyperintensities in the medulla oblongata, less so in the caudal pontine tegmentum, right cerebellar medulla, left posterior horn subcortical medulla, right insular/temporal medulla, around the temporal horns, right posterior cingulate and frontally on both sides. The imaging findings are consistent with limbic encephalitis.
Progression and therapy:
After the initial diagnosis, the patient was admitted to the neurological ward for further assessment. On admission, a saccadic gaze sequence, double vision and gait disturbance were also noted. Methylprednisolone shock therapy was administered over a period of 5 days. This treatment led to a slight improvement in the symptoms, in particular the saccadic gaze sequence and gait disturbance decreased.
Nevertheless, severe behavioural abnormalities continued to occur, such as reduced distance, sudden inexplicable fears and childlike behaviour. After positive NMDA receptor antibodies were detected in the cerebrospinal fluid, immunoadsorption was initiated over a total of 7 cycles. The patient subsequently developed a fever and was diagnosed with pneumonia. After antibiotic treatment, the patient's general condition improved.
During the infection-free interval, extended immunomodulatory therapy with rituximab was initiated in accordance with the guidelines. This was continued every six weeks for two years. As a result, both the psychological and neurological symptoms gradually improved.
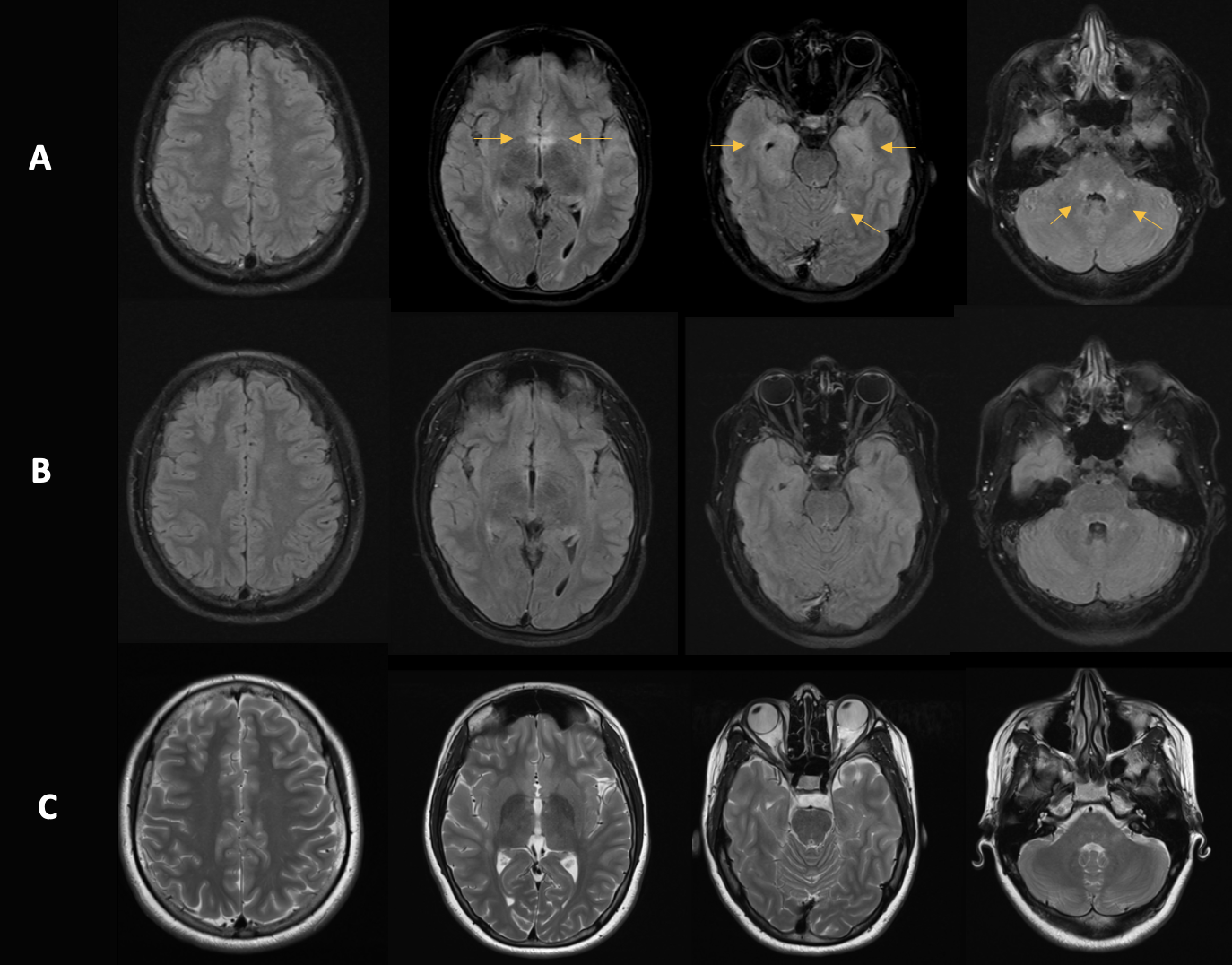
Figure 2: Follow-up using MRI
A: Initial imaging. B: Follow-up after 10 months. C: Follow-up after two years. There is a clear reduction in T2w hyperintensities over time, which correlates with clinical improvement.
NMDAR encephalitis, a rare and dangerous CNS disease
N-methyl-D-aspartate receptor (NMDA-R) encephalitis is an autoimmune disease characterised by the formation of antibodies against NMDA receptors in the brain. These receptors are essential components of synaptic transmission and play a central role in cognitive functions, learning and memory.
The disease was first described in 2007 and since then a deeper understanding of its clinical and pathophysiological aspects has been gained. Most patients are young women, and in many cases the disease can be associated with an ovarian teratoma, a tumour that often expresses NMDA receptors. Nevertheless, the disease can affect people of all ages and genders and can also occur without a detectable tumour.
Clinically, NMDA encephalitis often manifests with a non-specific viral prodrome, followed by psychiatric symptoms such as hallucinations, agitation, and paranoid behaviour. This phase may be followed by neurological symptoms, including impaired consciousness, movement disorders and seizures. Progression of the disease without treatment can lead to status epilepticus or coma.
Diagnosis is based on the detection of anti-NMDA receptor antibodies in serum or cerebrospinal fluid and is supported by clinical symptoms and imaging findings. Early diagnosis and treatment are crucial for the clinical course and outcome.
Therapy for NMDA encephalitis focuses on immunosuppression to reduce antibody production and control inflammation. First-line therapy often includes corticosteroids, intravenous immunoglobulin and plasmapheresis. In the event of an insufficient response, relapse or the presence of a tumour, more aggressive therapy with immunomodulators such as rituximab may be necessary.
Key take-away
As autoimmune encephalitis is usually accompanied by mental symptoms, it is often not taken seriously by non-experts. If behavioural abnormalities are detected alongside depressive moods, colleagues in medical practice and in outpatient settings should consider ruling out an organic brain cause for the mental symptoms using MRI.