In-hospitalization diagnostic procedure
During admission, the diagnostic procedure is completed to rule out an acute ischaemic event (TIA), a hypothesis arising from the transient nature of the focal disturbances.
An Angio-CT of the intracranial and extracranial vessels is performed. The examination shows regular calibre and course of the blood vessels, absence of stenosis, dissections or obvious vascular abnormalities.
This is followed by a transthoracic echocardiogram with microbubble test, which excludes right-left shunts or obvious interatrial defects. Prolonged electrocardiographic monitoring confirms a stable sinus rhythm, without significant arrhythmias or pauses.
Given the outcome of these examinations, the likelihood of a TIA is considered low.
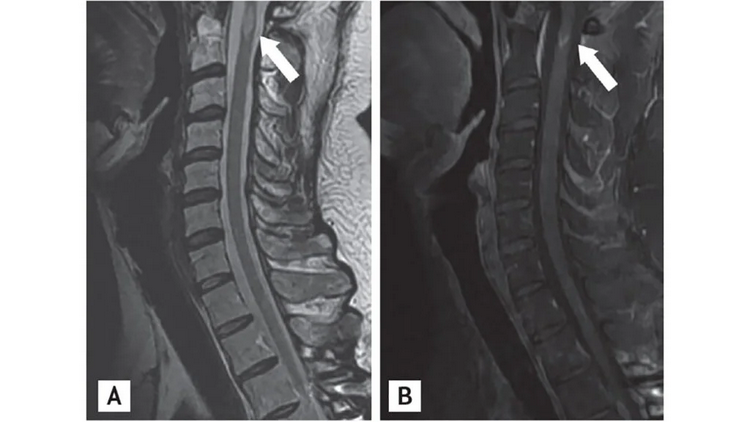
The patient is therefore admitted to the neurology department. Here the neurological evaluation with MRI of the brain and spinal cord with contrast medium is continued. This examination shows multiple periventricular, juxtacortical and infratentorial hyperintense lesions in T2/FLAIR. Some of these lesions enhance with contrast, others do not, suggesting dissemination over time. A single demyelinating lesion is present at the cervical level (C3-C4).
Lumbar puncture is performed, which shows the presence of intrathecal IgG oligoclonal bands (absent in serum).
Based on the McDonald 2017 criteria, the patient meets the criteria of:
- dissemination in space (lesions in ≥2 typical CNS areas);
- dissemination in time (capturing and non-capturing lesions, plus oligoclonal bands).
The definitive diagnosis is multiple sclerosis, relapsing-remitting form (RRMS).
Treatment and follow-up
The young patient starts disease-modifying therapy with subcutaneous interferon beta-1a.
The patient receives psychological and information support. Information about the disease is also provided to the young girl's parents. Outpatient follow-up with:
- MRI of the brain and cervical spine at 6 and 12 months;
- periodic neurological evaluation;
- annual screening for side effects of therapy.
Images of MS Lesions on the spine, via x ray. Image Credit: Yoon BN, Ha CK, Lee KW, Park SH, Sung JJ. A confusing case of multiple sclerosis and central nervous system graft versus host disease. Korean J Intern Med. 2016;31(5):995-998. doi:10.3904/kjim.2015.065
Take-Home Messages
- A new headache associated with focal neurological symptoms requires investigation even in young patients.
- TIA should be excluded with vascular imaging and cardiological evaluation, especially in cases with transient symptoms.
- Multiple sclerosis may begin with blurred symptoms, and early diagnosis is possible with the correct diagnostic work-up.
- Gadolinium-enhanced MRI and CSF examination are key tools to distinguish MS from other diseases (TIA, ADEM).
- Early treatment with DMTs can substantially change the natural history of the disease.