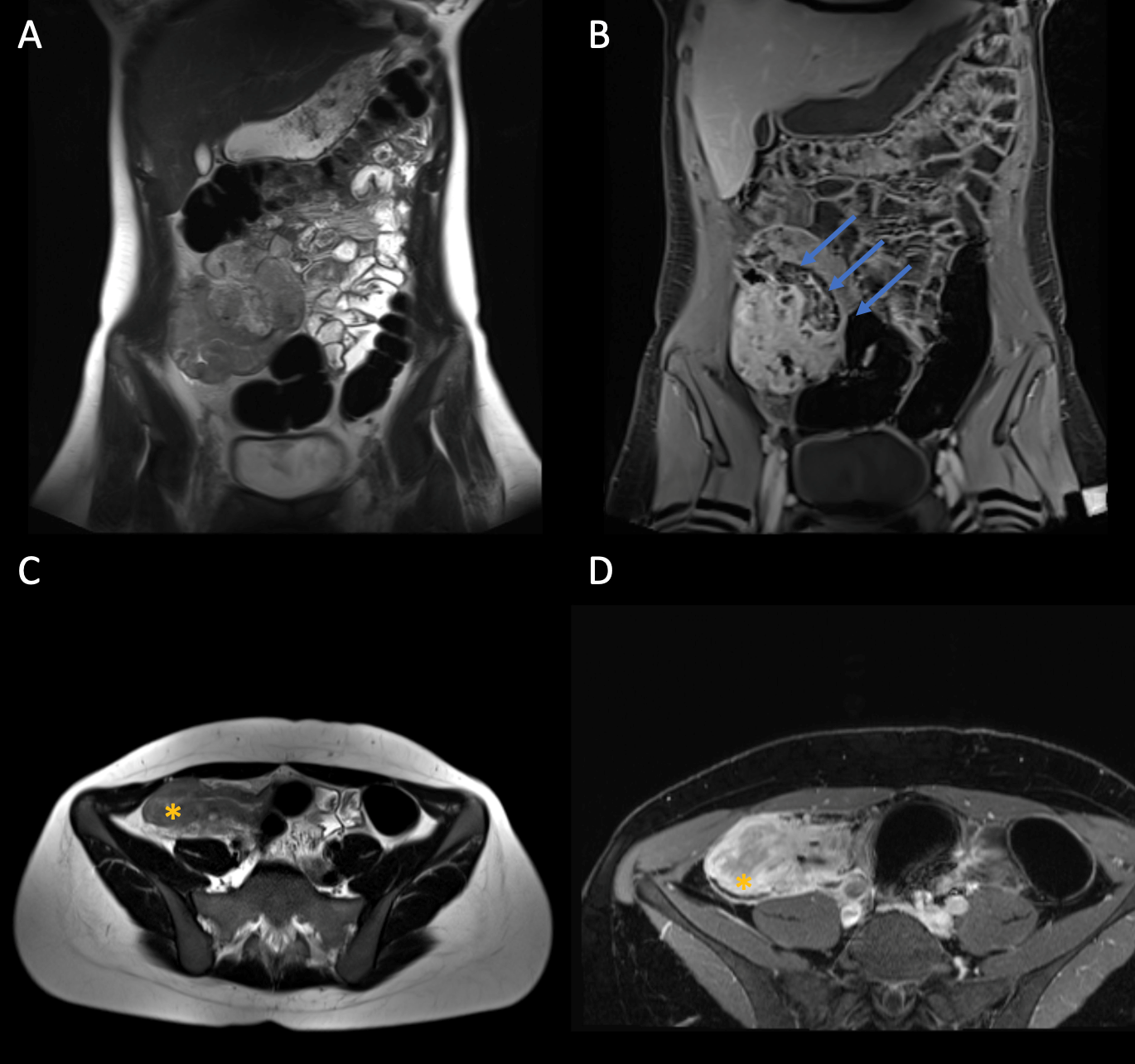
Figure (see above) A: coronal T2w HASTE. B: Coronal fat saturated (FS) T1w Post-KM . C: Axial T2w HASTE. D: Axial fat saturated (FS) T1w Post-KM. Blue arrow: Conglomerate tumour in the right lower abdomen. Star: Pronounced wall thickening of the terminal ileum.
Finding
The patient was diagnosed with terminal ileitis in Crohn's disease. Crohn's disease is a chronic inflammatory bowel disease (IBD) characterised by inflammation in various parts of the digestive tract. The inflammation usually occurs in the intestinal wall of the terminal ileum, but it can also occur in surrounding tissues (lymph nodes and fatty tissue) and lead to a conglomerate tumour, as is the case with Mrs M. Sometimes there is also fistula formation between the ileum and the urinary bladder or the ileum and the sigmoid.
The diagnosis of Crohn's disease is based on a combination of clinical symptoms, laboratory tests and imaging. The most common symptoms include abdominal pain, diarrhoea, weight loss and bleeding from the bowel. Diagnosis may involve a blood test to check for the presence of inflammatory markers in the blood. A colonoscopy should also be performed to assess the extent of inflammation and possible changes in the intestinal tissue. Sonography can be used to assess inflammatory activity according to the Limberg score. Magnetic resonance imaging is increasingly being performed as the gold standard to more accurately assess the extent of inflammatory changes and affected areas.
Therapy for Crohn's disease consists of controlling inflammation, treating symptoms, and preventing complications. Treatment is often with anti-inflammatory drugs such as steroids and immunosuppressants. In severe cases, biologics, antibodies or immunomodulators may be used. In addition, antibiotics may be used to treat infections and reduce inflammation. Dietary adjustments can also be made to reduce symptoms and prevent deficiencies. However, surgical options are often unavoidable in the advanced stages of the disease. Typically, an ileocecal resection is performed.
The prognosis of Crohn's disease depends on the severity of the disease and the effectiveness of therapy. With timely and appropriate treatment, remission can be achieved, with symptoms disappearing and the bowel remaining healthy. However, the disease can also recur and complications can occur, such as ileus or abscesses. Close cooperation between the patient and the doctor is necessary to slow down the progression of the disease and achieve the best possible prognosis. Since most patients tend to be affected at a younger age and treatment complexity is increasing, Crohn's patients are increasingly tethered to specialised centres and seen regularly.