Echinococcosis, a serious disease in agricultural regions
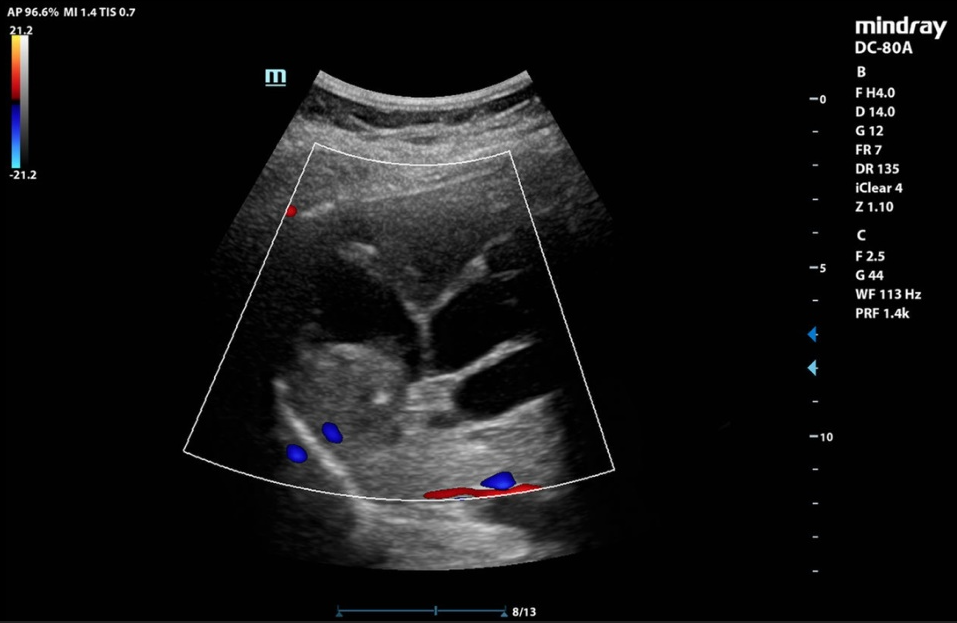
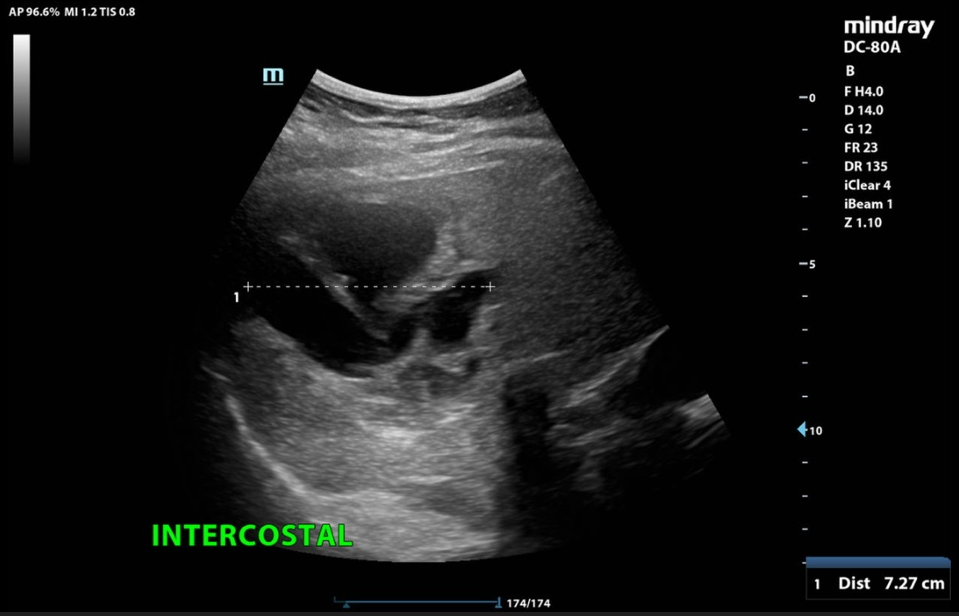
The CT scan showed a 16 x 14 cm multilobulated hypodense mass in liver segments VII, VIII and VIa, with consecutive cholestasis in the right liver lobe. The portal vein and the hepatic veins were open. The remaining organs were unremarkable. Serology for echinococcosis was taken for complicated liver cysts. When asked specifically about contact with dogs and foxes, Ms K stated that she had three dogs on the farm. The echinococcal IgG screening ELISA was positive at 47 U/ml. Thus the diagnosis of echinococcosis was made.
Echinococcosis, also known as tapeworm disease, is a rare but serious parasitic disease. It is caused by the larval stages of the tapeworms Echinococcus granulosus and E. multilocularis. Transmission occurs mainly through contact with infected dogs or foxes and through the consumption of contaminated food. The incubation period can be 6 months to several years.
In cystic echinococcosis (caused by E. granulosus), cysts form mainly in the liver and lungs and may remain asymptomatic until they reach a considerable size. In contrast, alveolar echinococcosis (caused by E. multilocularis) leads to tumour-like lesions that can spread infiltratively and affect other organs, such as the lungs and brain.
The development of the hydatidosis usually takes place over several years. After a long asymptomatic phase, patients give nonspecific upper abdominal symptoms up to icterus (in liver infestation), or irritable cough and thoracic tightness (in lung infestation). Rupture of an echinococcus cyst is a serious complication, as the leaking fluid can lead to anaphylactic shock, and the shedding of many new larvae can lead to the formation of new cysts.
Laboratory diagnosis is usually non-specific, and mild eosinophilia, thrombocytopenia and leukopenia may be seen. Detection may be done by use of immunodiagnostic tests such as ELISA, Western blot, or immunofluorescence antibody test. However, a negative serology does not exclude echinococcosis, because an increase in antibodies can be expected three months after exposure at the earliest.
Therapy is based on size, localisation and stage. It usually consists of a combination of surgical interventions and antiparasitic drugs. However, due to the often late diagnosis and complications, the prognosis remains serious. In the case of Mrs. K's extensive finding, preoperative embolisation of the right portal vein was performed to achieve proliferation of the left lobe of the liver. Three weeks later, an atypical resection of liver segments IV, VII and VIII was performed. The patient recovered rapidly and the jaundice was completely regressed. After the seventh postoperative day, the patient could be discharged home in good general condition.