Oh my sweet rhesus (a short history of blood transfusion)
Wars can have a few advantages, one of which is the advancement of medical practice. From 1914 to the Korean War, blood transfusion made great strides.
Every second, two people in the world give blood. But it took a long time for blood collection and transfusion to become the safe and controlled process we know today. A look back at the long history of blood transfusion. In this article, Jean-Christophe Piot relates with a certain rigour - and a certain freedom of tone - the most significant pages in the history of medicine.
Made in cooperation with our partners from esanum.fr
"The heroism of a physician. To save a dying woman, a surgeon from Bordeaux injects her with his own blood" (Le Petit Journal illustré, 1921). This drawing illustrates the article recounting the intervention of Dr. Corbin, a physician at the Bordeaux General Hospital, who gave his blood to a woman 'who was dying of haemorrhage'.
We would be remiss if we didn't mention it: One of the earliest literary references to blood transfusion comes from Bram Stoker's Dracula. Published at the very end of the 19th century, the novel constantly plays on the opposition between the gothic darkness embodied by the old vampire on the one hand and the wonders of science on the other. The dark designs of the Count are opposed by the lights of knowledge, personified by the good Doctor Van Helsing. And it is the latter who attempts a last-chance transfusion on Lucy, a young woman who wakes up more and more bloodless every morning.1
On several occasions the doctor performs the transfusion in the proper manner: "As he spoke, Van Helsing was already taking the instruments for the transfusion from his kit; I had taken off my jacket and rolled up my shirt sleeve and without missing a moment, we proceeded with the operation. After a few moments, which did not seem short to me, for it is painful to feel that your blood is running out of your veins even if you give it willingly, Van Helsing held up a warning finger…”
Stoker's use of the term "operation" is particularly apt: In 1897, when the novel was published, transfusion was still done "live", if you will, or more precisely from arm to arm. To replace Lucy's lost blood, Van Helsing performs a genuine surgical operation by cutting the veins of his patient and several of his companions. Painful, but arguably preferable to the whole blood donation that Dracula and all his pop culture pals tend to demand.
If Stoker stages this episode, it's because he knows it will leave a mark on his readers. At the time, the very idea of giving blood was not at all trivial. Yet transfusion was about to take a decisive step forward at the dawn - Dracula would appreciate it - of the 20th century. The first attempts at transfusion date back a good three centuries, but these beginnings were, how can I put it, complicated.
Reversing the logic of bloodletting
It has to be said that as soon as we talk about blood, everything gets complicated. Even today, the symbolic weight associated with it remains impressive, whereas in the 17th century... Physicians at the time had long since considered blood to be one of the four "humours" that govern human health, along with phlegm, yellow bile and black bile. Since ancient times, illness in the broadest sense has been interpreted as an imbalance of these humours, and the physician's art has been to remedy it with purgatives, enemas and bloodletting. Therapeutics somewhat mocked by Molière in Le Malade imaginaire: "... I would let him die without help. No matter what he does or says, I would not order the slightest bloodletting, the slightest enema..." (Argan, act III, scene III).
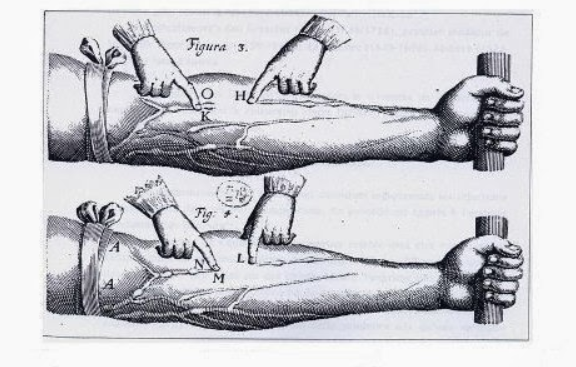
It was in the 17th century that the idea of a principle diametrically opposed to that of bloodletting emerged. What if it was useful to inject blood into a patient rather than withdraw it? The German physician Andreas Libavius was the first to envisage what was not yet called a transfusion. "Let us take a robust young man, in good health and full of vigorous blood: Let another, exhausted of all his strength, thin, emaciated and with panting breath, be held by his side; let the man of art have silver tubes fitting each other; let him open an artery of the robust subject, insert a tube and hold it there; let him immediately open an artery of the sick man and insert the other pipe; then let him fit the two pipes together and let the blood of the healthy man rush, warm and vigorous into the sick man, bringing the source of life and driving out all weakness."
Put like that, it sounds simple. But there were still some slight technical, anatomical and scientific problems to be solved. The hardest was probably to get the physicians to agree on a new theory of blood circulation made in England. In 1628, William Harvey's Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus (for non-Latin speakers: "Anatomical exercise on the movement of the heart and blood in animals") was published.
"Well, guys, aren't you about to finish fiddling with my valves?
Harvey's predecessors and contemporaries believed that blood was constantly being reformed from digested food and that the primary function of the heart was heat production. De Motu Cordis provokes one of the greatest medical barbs of the 17th century because it changes the perspective quite a bit by showing that the heart muscle functions as a pump. Basically, Harvey explains that by observing animals he found that systole was the active phase of the heart's movement and that the quantity of blood leaving the heart was too great to be absorbed by the tissues. It was a good thing: Fabricius, his professor in Padua, had discovered the presence of valves in the veins. Conclusion: "... I began to think that it [the transmission of blood] might rather have a certain movement, so to speak, in a circle (...) through the heart, the blood is sent to the whole organism, passes through the porosities of the tissues, returns through the veins of the extremities towards the centre to end up in the right heart atrium".
The scandal broke out between opponents and supporters of Harvey's thesis. In France, it took a good fifty years before Louis XIV blew the whistle on the controversy by obliging the university to teach the English theory. In the meantime, the technical possibility of performing a transfusion had progressed thanks to another Englishman, an architect to boot. When he was not on the building site of St. Paul's Cathedral in London, Charles Wren kept himself busy by inventing the first devices capable of allowing the intravenous injection of various liquids in liquid form - including blood, therefore. Two English trials, one might say, but the transformation was to be... French.
First attempts
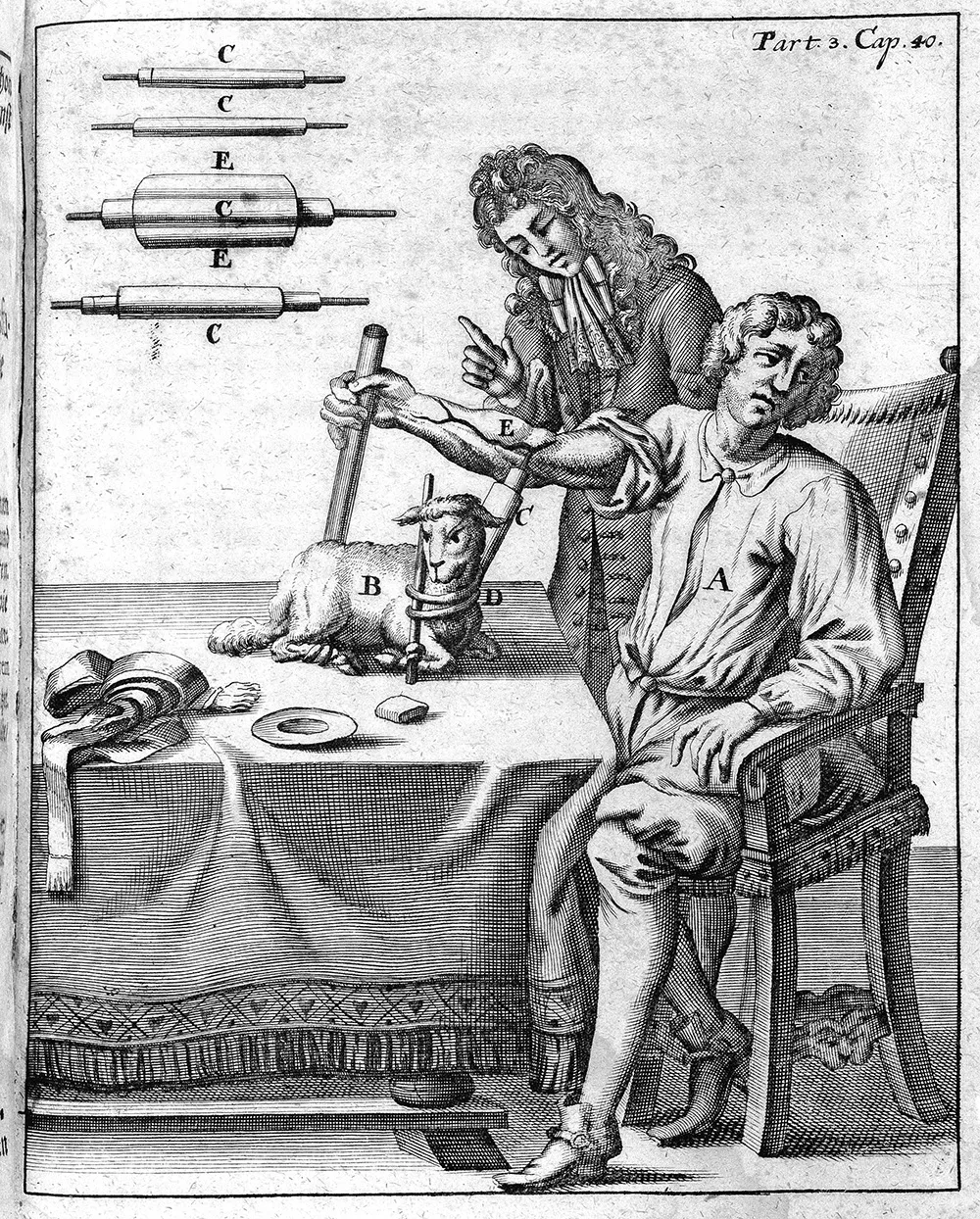
The first practitioner to try this was not just anyone: It was the Sun King's physician, Jean-Baptiste Denis. He first practised by putting unfortunate mutts who had not asked for anything through a lot of hassle. The first transfused human being in history was a 15-year-old boy, exhausted by the fifteen bloodletting sessions he had undergone in the previous weeks. At five o'clock in the morning of 15 June 1557, Denis took a little more blood from him. He removed three ounces of blood by opening a vein in his elbow, which was immediately replaced by the injection of nine ounces (about 270 centilitres) of blood... from a lamb, properly bled at the carotid artery. Why a lamb? Simply because of its reputation as a gentle and kind animal.
"Gentle and nice", you don't have to push it...
We now know that statistically, a blood donation between two human patients made without taking into account their blood type would cause serious problems in a third of the cases. We can hardly imagine the figures with a xenotransfusion, but Denis obviously has no idea of the existence of blood compatibilities, nor does he have the tools to understand the principle of haemolytic shock. The young patient, undoubtedly blessed by the gods, nonetheless comes out of it like a flower, or almost - he will only complain of a great heat in his whole body. The same goes for the second patient. If the third patient dies quickly after the injection, the cause of his death has nothing to do with the transfusion itself.
Dare we call it a success? The competition between France and England is still raging. If Denis opened the score on 15 June 1667, two Englishmen - Lower and King - replied on 23 November of the same year with a very similar transfusion. Ironically, Denis presented the very first transfusion in the form of a letter written, in English, to the leading scientific institution: The Royal Society.
But back to his patients. The fourth transfusion recipient was to put a stop to transfusion by suffering the first fatal haemolytic accident in history in December 1667. Unable to understand what was happening before his eyes, Denis could only see the damage when the body of Antoine Mauroy, a 34-year-old servant, began to reject the blood cells3 of an obviously incompatible donor - in this case a calf. During his third transfusion session, his pulse skyrockets, he sweats, cries, shakes and clearly suffers martyrdom before dying in the night. Already, after his second transfusion, Antoine Mauroy had shown some alarming signs, including an intense lumbar pain and the emission of black urine, according to Denis, "as if it had been mixed with soot".
His widow cried murder and even though Denis was cleared in the ensuing trial4, the Châtelet court issued a ruling in April 1668 that recognised the success of previous attempts but concluded that it might be necessary to stop engaging in bizarre experiments: "From now on, it is strictly forbidden for any person to carry out transfusions on any human body unless the proposal has been received and approved by physicians from the Paris faculty, on pain of imprisonment". Given the rather conservative positions of the faculty in question, it was a first-class burial that the Paris parliament confirmed two years later: "All physicians and surgeons are forbidden to practice blood transfusion on pain of corporal punishment and imprisonment. Extraordinary tests are generally dangerous: and for one that succeeds, all the others become fatal”. Wracked by similar failures, England followed suit a few months later.
Adventurous 19th century
The end of the line? No. After several decades of interruption, transfusion returned to the forefront in 1818 thanks to the English obstetrician James Blundell, who was distraught to see women in childbirth slamming into his hands frantically because of haemorrhages that the medical profession was having trouble stopping. The physician thinks he can avoid the problems encountered by his predecessors by choosing the person closest to the patient as a donor, namely the husband. The logic is worth what it is worth: If the father gave life with the "white blood" that came out of his glorious genitals, he can save his wife with his red blood. Well, why not.
Blundell attempts the operation on women who are in a desperate state anyway and the successes he achieves, when the blood types of the two spouses have the good sense to be compatible, impress the scientific world. The obstetrician also made remarkable progress on the technical front. He devised a series of injection devices, each more appropriate than the last, including syringes and the "gravitator", a support placed above the patients to facilitate the injection of the liquid by playing on gravity. On the other hand, he came up against a recurring problem that made his life difficult: Coagulation greatly reduced the window of opportunity. Any transfusion is a race against time.

The famous 'gravitator', or the art of adding gravity to a situation that has plenty of it.
The faithful ABO is born
A major step was taken in 1900: The Austrian biologist Karl Landsteiner had the excellent idea of identifying blood groups, which were codified in 1909 in the ABO system that we still know today. This reduced the risk of transfusion shock to (almost) zero and led to a Nobel Prize in 1930. The scientist perfected his discovery in 1940, when he discovered the two antigenic erythrocyte systems for rhesus+ and rhesus-. Eternal glory to the Rhesus macaques (Macaca mulatta), who gave their name to this system.
Between these two discoveries, 1900 and 1940, the First World War served a rare purpose: To advance transfusion by leaps and bounds. Until the beginning of the 20th century, transfusion remained an exceptional and complex surgical act, of which Bram Stoker's text, mentioned above, is a fine illustration. Everything is done from arm to arm, generally from artery to artery, to make a direct donation. Not only does it hurt, but it has been simpler in the past. Fortunately, the great slaughter of the First World War changed all that. With the explosion in the need for blood on battlefields where there was no shortage of donors or recipients, research progressed. A Belgian physician, Albert Hustin, had the good idea of solving the problem of coagulation by adding sodium citrate to blood to keep it fluid. Other discoveries made it possible to store and transport donations in glass jars.
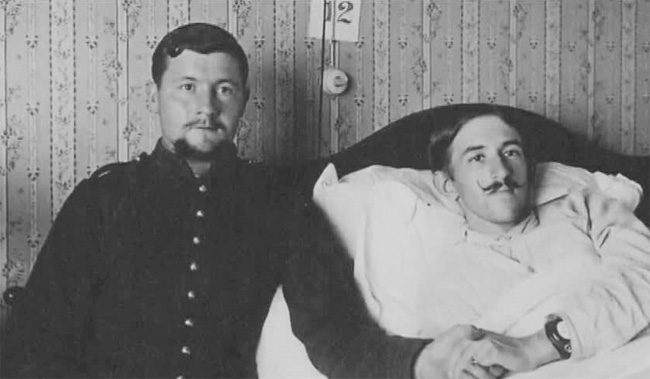
The first of 44 transfusions in 1914.
Some convalescent hospitals were set up in hotels in the seaside resorts of southern France. Because of the distance involved, the wounded could arrive at these hospitals in a state of exhaustion. In Biarritz, the artilleryman Isidore Colas gave his blood to Corporal Henri Legrain so that he could undergo amputation. He died in 1987, aged 98.
The birth of modern transfusion
In the aftermath of the First World War, blood transfusion became structured in every respect. In 1923, the French physician Arnaud Tzanck created a "Blood Transfusion Society" in Paris, which established a principle that has remained unchanged: Donation is free of charge and is considered to be an act of devotion that can never give rise to remuneration. Little by little, transfusion became commonplace. In 1931, the Assistance publique de Paris had 500 donors. The number of transfusions rose from 200 in 1929 to 3,700 three years later.
England and the United States followed similar paths and came up against the same obstacle: The storage of haemoglobin. Projects for blood banks were discussed at international congresses, the first of which was held in Rome in 1935. The same year, blood banks appeared in the United States, one of which was created by the surgeon Carl W. Walter. Why him? Because during his studies he witnessed a direct transfusion, in the operating theatre, between a donor and a patient undergoing a craniotomy. As the patient's condition deteriorated, the pressure in the tubing increased until it exploded. Walter then thought - gosh darn it - there had to be another way.
To house this blood bank, Walter chose a room in the Harvard basement. Let's just say that some administrators felt that the storage and use of human blood was unethical at the time. The blood was still stored in hermetically sealed glass vials for no more than ten days. Another innovative attempt to transfuse blood from the recently deceased to the sick soon failed.
Like the first, the Second World War boosted research and innovation on transfusion, which once again became a priority on the battlefield. All the belligerents set up services capable of providing transfusion care for the wounded, whether civilian or military. The 1940s and 1950s saw the development of modern transfusion in three stages. In 1940, the American Edwin Cohn succeeded in fractionating plasma and its various proteins, thus enabling the preparation of albumin. Three years later, the Englishmen Loutit and Mollison developed the "ACD" preservation solution for citric acid, citrate and dextrose. This extended the storage time for blood to three weeks. Finally, Walter - again - and his colleague Murphy designed the first plastic blood bag. This revolutionary technology, tested during the Korean War, would take more than twenty years to replace the good old glass bottles before becoming the standard.
Since then... Let's just say that we're tinkering with technologies that were already well established, with the development of platelet concentrates in 1963, the development of blood cell separation by apheresis in 1973 or the discovery of additive solutions for red blood cell concentrates in 1978. The rest is a general strengthening of transfusion safety through a series of ever more advanced biological controls - from the search for pathogens to the faster determination of blood groups - in order to constantly improve the safety of donors, recipients and caregivers. This enables the collection of almost 120 million donations per year, all over the world.
Notes:
1. And for good reason, it's been serving as Dracula's fast-food restaurant for a few nights already when Van Helsing finally reveals what's going on to his incredulous entourage, before hanging 200 kilos of garlic in the windows and sticking crucifixes everywhere. We won't tell you the rest.
2. "Plus, from the twenty-fourth, a small insinuating, preparatory and emollient clyster, to soften, moisten, and refresh the bowels of Monsieur (...) and the other month there were twelve medicines, and twenty enemas."
3. Still unknown to Jean-Baptise Denis: It was not until 1674 that the Dutchman Antoni Van Leeuwenhoek described the composition of blood for the first time in these terms: "I observed the blood in my hand and found that it consists of red blood cells swimming in a clear liquid.
4. Where it is not a question of contaminated blood, but of "pernicious blood".