The long view: visual acuity threatened by advancing age
Glaucoma, diabetic retinopathy and age-related macular degeneration are among the diseases that threaten visual acuity.
Ophthalmology
By Dr. Annabelle Eckert
Glaucoma, diabetic retinopathy and age-related macular degeneration are among the diseases that threaten visual acuity
The importance of vision for the human organism is reflected in the anatomy of the central nervous system, as 40% of afferent nerve fibers originate from the eyes. Glaucoma, diabetic retinopathy and age-related macular degeneration are among the diseases that threaten visual acuity (Sources 1, 2).
Age-related macular degeneration
Age-related macular degeneration (AMD) is a progressive disease of the elderly population and is associated with an increasing central reduction in visual acuity. It is responsible for around 50% of blindness cases in Germany (Source 3).
The DALYs (see Fig. 1) is a calculation model used to illustrate the relevance of AMD compared to other common diseases. The score is calculated by multiplying age by the degree of physical limitation. According to epidemiological estimates, AMD will continue to gain in importance for the population until 2030, when it will be a burden of disease (Source 3).
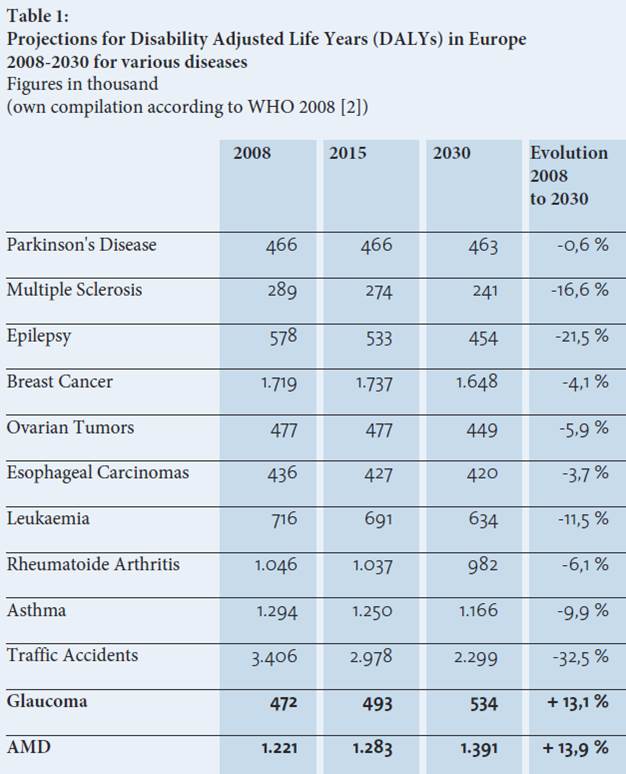
Figure 1: Projections for Disability Adjusted Life Years (DALYs) in Europe (Source 2, Image translation by editor).
Epidemiology of AMD
In Germany alone, around 1,608,000 people will be affected by AMD in 2012. It is estimated that this number will increase further to 2,131,000 in 2030 (Source 3). In America, around 10 million people suffer from age-related macular degeneration. The number of AMD patients is thus twice as high as the number of Alzheimer's patients (Sources 4,5).
Loss of reading ability
AMD prevalence increases steadily with age. Only rarely are young patients affected (2% of 40-year-olds). Light-skinned patients of the female sex are, particularly at risk. Dry AMD is a chronic progressive disease that can lead to blindness of the central visual field if left untreated. Patients lose the ability to read and recognize faces.
Stages of the AMD
In the early stages of AMD, insoluble extracellular aggregates, drusen, accumulate in the retina. (Bird, 2010). The late stage of dry AMD is characterized by confluent or scattered degeneration areas of the retinal pigment epithelium (RPE). Without the RPE that supplies them, the photoreceptors also perish. Because of its morphology, it is also called geographical atrophy. 10-15% of AMD patients suffer from exudative AMD. She's the more aggressive form of the disease. The wet form of AMD often develops on the soil of the dry AMD disease.
Pathomechanism of AMD
The phagocytic function of the retinal pigment epithelium decreases with age. The result is lipofuscin deposits in the RPE cells. Drusen formation occurs in the region of the fracture membrane, or more precisely in its extracellular matrix. This and a diffuse membrane thickening lead to an undersupply of the RPEs. The result is hypoxia with a secretion of VEGF (vascular endothelial growth factor) by the RPE cells. Antigen-presenting and phagocytically active cells (macrophages and dendritic cells) are attracted by the oxidized fraction membrane components.
Choroidal neovascularization
Exudative AMD is distinguished from dry AMD by the presence of choroidal neovascularization (CNV). The neovascularizations reach the retinal layers after breaking through the fracture membrane. Leakage from abnormal blood vessels can result in fluid accumulation. The affected patient notices this as metamorphopsia. Bleeding and scarring can result in rapid vision loss (Source 6). Modern diagnostic and therapeutic procedures (intravitreal injections, dietary supplements) have given patients hope in recent years because the disease process can be slowed down. We will discuss the various therapy modalities in more detail in the other blog posts.
Healing in sight?
A current study is investigating the use of a biologically designed composite implant (California Project to Cure Blindness-Retinal Pigment Epithelium, Source 1). This consists in part of a polarized monomolecular RPE layer derived from human embryonic stem cells. This layer rests on a synthetic parylene layer, which is modeled on the fracture membrane.
The implant was successfully inserted in 4 of the 5 study patients. Using OCT (optical coherence tomography) diagnostics, the correct use of the implant was tested and integration of the new photoreceptors was confirmed. The 4 successfully implanted study participants showed no further reduction in visual acuity during the course of the study. One of these patients even showed a gain of 17 letters. Improved fixation was observed in two study eyes.
A very interesting and innovative study. The question arises as to whether she can lay the foundation for healing? We are eagerly awaiting the long-term results.
Sources:
1.Ambati J. et al. (2012). Mechanisms of age-related macular degeneration. Neuron. 75 (1): 26-39.
2.http://www.dog.org/wp-content/uploads/2013/03/DOG_Weissbuch_2012_fin.pdf
3. Finger, R. P. et al. (2011). The incidence of blindness and severe visual impairment in Germany: projections for 2030. Invest Ophthalmol Vis Sci, 2011. 52(7): p. 4381-9.
4. Friedman D. S. et al. (2004). Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004;122:564–572.
5. Brookmeyer R. et al.(2007). Forecasting the global burden of Alzheimer’s disease. Alzheimers Dement. 2007;3:186–191.
6. Färber L. et al. (2010). Medizinische Spitzenforschung in Deutschland. Schattauer. 41-42.
7. Kashani A. H. et al. (2018). A bioengineered retinal pigment epithelial monolayer for advanced, dry age-related macular degeneration. Sci Transl Med. 10(435).