Updates on coeliac disease diagnosis in children
A free, online decision-making algorithm helps physicians with diagnosis, evaluation and treatment for coeliac disease management in pediatrics.
About celiac disease
Coeliac disease is defined as a permanent immune-mediated response to gluten, a protein complex found in various wheat, barley and rye foods. Coeliac disease has a wide spectrum of clinical manifestations that make it closer to a multisystem disorder rather than an isolated intestinal disease. It is characterised by lesions of the small intestine and the presence of specific antibodies. The detection of specific antibodies for coeliac disease (e.g. anti-tissue transglutaminase, anti-gliadin antibodies) in serum is very useful for the initial screening of patients with suspected disease.
The gold standard of diagnosis is the histological examination of the small intestinal mucosa, so an intestinal biopsy is required to confirm the diagnosis. The current treatment of coeliac disease requires strict adherence to a gluten-free diet (GFD) and lifelong medical follow-up. Most patients have an excellent clinical response to GFD.
The estimated prevalence of coeliac disease is around 1%. Coeliac disease diagnosis rates are on the rise. The most recent increases in coeliac disease diagnoses are probably due to increased awareness, although research has shown that the prevalence of the disease has increased in recent decades for unclear reasons.
The popularity of the gluten-free diet creates difficulties in identifying whether individuals with symptoms attributed to gluten are actually suffering from coeliac disease.
An online tool for a difficult diagnosis
A few years ago, the Celiac Disease Foundation and the North American Society for Paediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) jointly developed the NASPGHAN Clinical Guide for Paediatric Celiac Disease, an evidence-based decision-making algorithm using a probability system derived from the literature.
The clinical guide consolidates the latest research, guidelines, and expert opinion into an easy-to-use and intuitive tool to help clinicians interpret test data, simplify diagnoses, and improve the quality of care they are able to provide to patients with celiac disease.
This free guide aims to help physicians untangle some of the most challenging elements of the approach to caring for patients, particularly children, who may have celiac disease.
The diagnosis of paediatric coeliac disease can be challenging. The signs and symptoms of the disease vary from gastrointestinal, such as abdominal pain, diarrhoea or constipation, to extraintestinal, such as asthenia, poor growth or delayed pubertal development. Symptoms may be mild, intermittent or absent.
Furthermore, although positive coeliac serology, such as anti-transglutaminase IgA (tTG-IgA) and anti-endomysium IgA antibodies, are good predictors of the diagnosis of coeliac disease, even children without this condition may have a positive diagnosis of coeliac disease. Therefore, the gold standard diagnostic test is a biopsy of the small intestine before starting a gluten-free diet.
An up-to-date decision-making algorithm
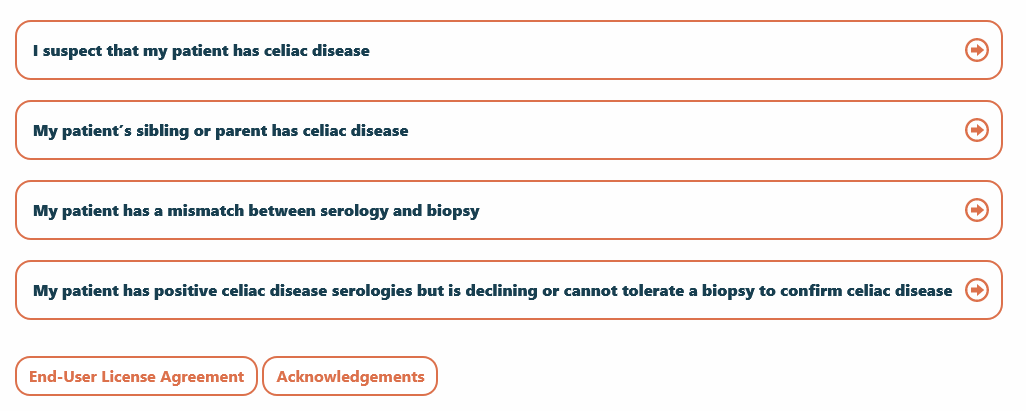
To help physicians choose between different courses of action based on the patient's history, signs and symptoms, the branches of the decision tree start from four nodes, which initiate the decision paths for patients with:
- Suspected coeliac disease.
- A sibling or parent with coeliac disease.
- Mismatch between serology and biopsy.
- Positive serological results for coeliac disease that refuse or cannot tolerate a confirming biopsy.
Each of these starting points leads to further branches of the decision tree. For patients with suspected coeliac disease, for example, the system asks whether the patient continues to consume gluten without restriction. If the answer is yes, the guide recommends testing for coeliac disease with TTG-IgA and total serum IgA. The results of these tests become internodes leading to other branches. If the answer is negative, the guide asks physicians to assess whether the patient is able and willing to tolerate a gluten challenge, and leads to other internodes and decision branches.
Below is a visual sample of the algorithm user experience:
Following the pathway for the suspicion of coeliac disease in patients who continue to consume gluten and have a positive test for coeliac disease, endoscopy with duodenal biopsy for the detection of lesions according to the Marsh-Oberhuber classification is recommended. The result of the biopsy determines how to proceed with the algorithm.
In a symptomatic patient who refuses or cannot tolerate a confirmatory biopsy, recommendations depend on the TTG-IgA titre results. For example, if the titre is greater than 10 times the laboratory's upper limit of normal, a test for endomysial IgA antibodies is recommended, followed by a test for a risk gene for coeliac disease if the endomysial IgA antibody is positive.
A patient with a positive gene test in this scenario meets the criteria for a serological diagnosis of celiac disease. Each screen of the interface includes relevant literature to support the guidance.
Atypical scenarios can challenge even the most experienced doctors
With the increase in paediatric diagnoses of coeliac disease in recent decades, and the fact that it is a chronic condition, paediatricians should be familiar with the typical and atypical presentations of the condition and how to diagnose and treat its complications.
Paediatric gastroenterology physicians are familiar with coeliac disease and know how to diagnose it. However, questions may arise in less common scenarios, such as a mismatch between serology and histology or patients who have already started a gluten-free diet before considering testing for celiac disease. Each of these scenarios can represent a diagnostic dilemma and, in some cases, this tool can guide physicians towards potential strategies that may lead to a more definite diagnosis for the patient.
The tool's developers envisage it for being used primarily by paediatric gastroenterologists and other physicians working in this field as a reference when encountering difficult cases. The aim is also to reach family paediatricians, so as to standardise the diagnostic approach to this condition. The end result of this work should be a further step forward in the diagnosis of coeliac disease and the restriction of the gluten-free diet for children who have not been appropriately evaluated.
