The ERC Guidelines 2021: Adult Advanced Life Support (Part 3/7)
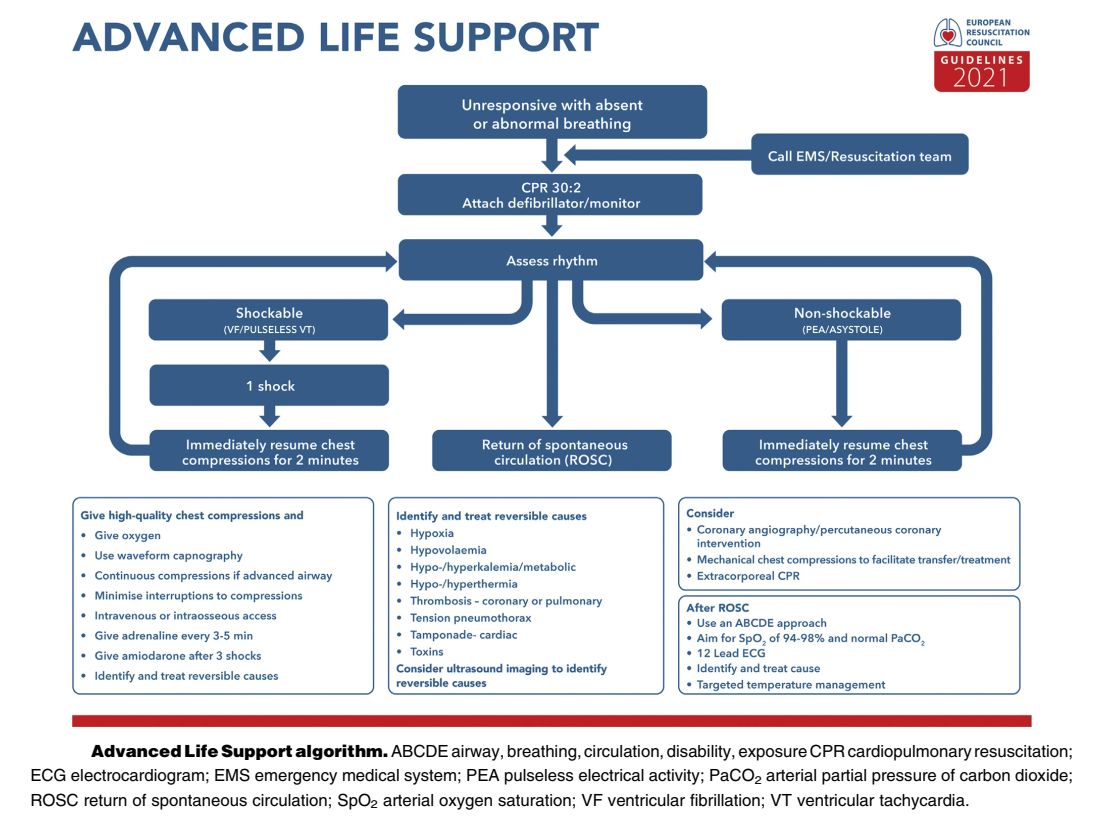
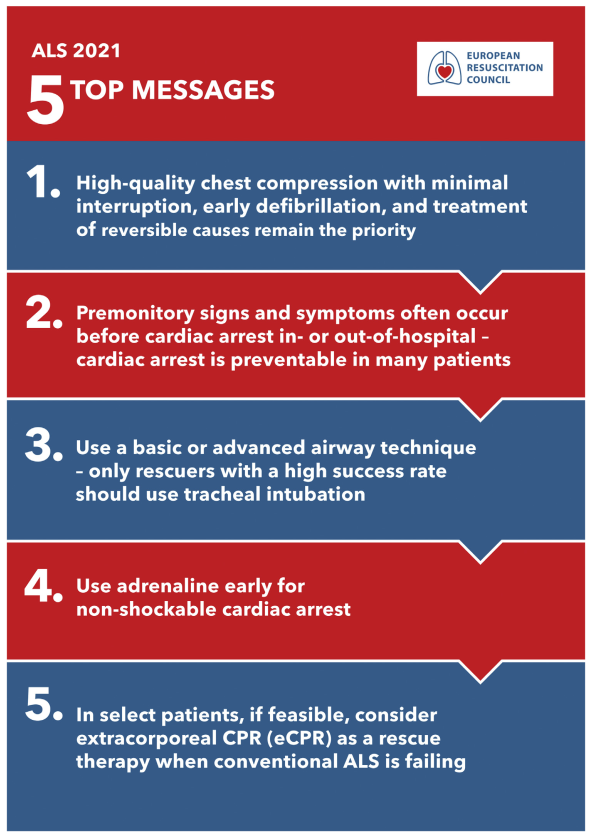
The five key points of the ALS 2021 procedures are: chest compressions and early defibrillation, warning signs of cardiac arrest, endotracheal intubation, use of adrenaline, and ECPR.
There are no major changes in the adult advanced life support (ALS) guidelines
The five key points of the adult advanced life support (ALS) 2021 procedures are: chest compressions and early defibrillation, warning signs of cardiac arrest, endotracheal intubation, use of adrenaline, and extracorporeal cardiopulmonary resuscitation (ECPR).
Made in cooperation with out partners from esanum.it
There is a greater acknowledgement that patients with cardiac arrest have warning signs and that many of these arrests are preventable. Another key element is the focus on high quality compressions, always with minimal interruptions, and early defibrillation. With regard to the airway, endotracheal intubation is only recommended if the person applying it is experienced in performing the procedure (high success rate).
When adrenaline is used, it should be used as soon as possible. Guidelines report increasing evidence of ECPR as a treatment for selected patients under cardiac arrest when conventional measures are not effective, or to facilitate specific interventions (e.g. percutaneous transluminal coronary arteriography and angioplasty, pulmonary thrombectomy for massive pulmonary embolism, rewarming after hypothermic cardiac arrest) in settings where it can be implemented.
Below is a summary of the new elements (and some confirmations) prepared by Dr. Martin Fandler (Sozialstiftung Bamberg, Bamberg, Germany):
Drugs and their access
Amiodarone and lidocaine
- Are equivalent in Ventricular Fibrillation (VF) / Ventricular tachycardia (VT).
- After the third shock: amiodarone 300 mg or lidocaine 100 mg iv/io.
- After the fifth shock: amiodarone 150 mg or lidocaine 50 mg iv/io.
Intravenous access
There is weak evidence of worse outcomes with drug administration via intraosseous (i.o) access than with intravenous (i.v.) access. If i.v. access is not available (quickly), the procedure for i.o. access is performed.
Adrenaline recommendations
- For non-shockable rhythms (Pulseless electrical activity or PEA, asystole): 1 mg iv/io as soon as possible, then every 4 minutes.
- For defibrillation rhythms (VF/VT): 1 mg iv/io after the third (unsuccessful) shock, then every 4 minutes.
Thrombolytics administration
- Do not administer thrombolytics routinely.
- Consider thrombolytic drug therapy only if the suspected/confirmed cause of cardiac arrest is pulmonary embolism.
- After administration of thrombolytic drugs, CPR manoeuvres should be continued for at least 60-90 minutes.
Fluid administration
- No routine fluid administration.
- No routine administration of 'large' volumes of fluid unless the cause of arrest is clearly hypovolemia (oligemia) (which for the 2021 guidelines remains as an unchanged recommendation, emphasised again this year).
Defibrillation
It is recommended to shorten the 'waiting time' until the defibrillator is charged: even a 5-10 second pause reduces the chance of a successful shock. A primary recommendation sequence is 1. rhythm control 2. shockable rhythm 3. continue compressions until the defibrillator is charged, 4. apply shock (with the shortest possible pause). Alternatively, this is referred to as 'pre-charging'. The defibrillator can be charged already during a compression and is therefore immediately available during rhythm control (however, there is no sufficient evidence for this method although it is potentially a good option for trained teams, and safety aspects need to be assessed).
The use of defib-pads (adhesive plates) only is recommended. The positioning of the pads remains unchanged, but it is formulated more precisely. The "standard" position is anterolateral (sternal-apical):
- Right plate: to the right of the sternum, below the clavicle ("right side up").
- Left plate: approximately at the level of the V6 electrode, as far to the side as possible ("under the armpit") and not on the chest.
Other possible positions are antero-posterior (anteriorly at the apex of the heart, posteriorly behind the heart and under the scapula) and bi-axillary (under the armpit on both sides). If there is an implantable cardioverter-defibrillator (ICD)/pacemaker, the pads should be placed at least 8 cm away from the implant, and hence if necessary the treating person should choose an alternative position (see above). The anteroposterior position may be more effective for cardioversion of atrial tachycardia. In fact, both anterior-posterior and antero-lateral 'standard' positions are recommended. As of the 2021 guidelines, there are no recommendations yet for hands-on defibrillation.
The rhythm must be checked as soon as the defibrillator is ready, then every 2 minutes. If the rhythm is shockable, shock, do not pause, and continue chest compressions immediately. Only in the event of a VF/VT arrest observed on the monitor, use a three-shock strategy (up to 3 shocks in quick succession) if the defibrillator is available immediately.
With regard to the energy to be used, the recommendation is unchanged. For biphasic waveforms (rectilinear or truncated exponential waveforms), deliver the first shock with an energy of at least 150J. For pulsed biphasic waveforms, deliver the first shock at 120-150 J. Evidence suggests "lower" initial shocks (150J biphasic), then increasing current levels with each subsequent shock.
In case of persistent ventricular fibrillation, there are no recommendations for dual shocks. It is recommended to check the position of the defibrillator pads, and to change their position if necessary (e.g. from sternal-apical to anterior-posterior).
Airway management
There are yet no clear indications to determine an algorithm that can hint at a preferred method for ventilation. The pros and cons of various procedures [Ambu bag (Bag valve mask) , Supraglottic airway devices (SADs), endotracheal intubation] are indicated in the guidelines.
One would think, therefore, that ventilation at an early stage is not drastically important for the final outcome. For experienced teams ("high intubation success rate") there is a choice between SADs and intubation. Less experienced teams ("low intubation success rate") should use a SAD. Unfortunately there at present no clear recommendations for videolaryngoscopy.
Editor’s comment: Apart from experienced teams who can handle immediate intubation, the following procedure seems pragmatic/wise: immediate supraglottic airway (SGA) device, then intubation to return of spontaneous circulation (ROSC). In case of prolonged CPR, asphyxia and especially with the use of mechanical CPR devices (MCPR), endotracheal intubation should be used if possible, and always if there is availability of a videolaryngoscope, or capnography.
Once the endotracheal tube or SGA device is inserted, chest compressions should be performed continuously (with 10 ventilations per minute). With a SGA device, leakage should be checked and, if necessary, a 30:2 compression-ventilation ratio should be used.
Editor’s comment: Especially with an SGA device and continuous chest compressions, constant and frequent monitoring of tidal volume is necessary. Especially if the combination of laryngeal mask + mechanical chest compression is used, should there be any doubt about adequate ventilation, consider the 30:2 compression-ventilation ratio or monitor closely.
Continuous capnographic monitoring is recommended to check the position of the endotracheal tube, for quality control of resuscitation and detection of sudden ROSC. The trend of End-tidal CO2 (EtCO2), rising during the course of potential ROSC or falling during failed resuscitation, may be more useful than individual numbers. Falling EtCO2 values may also indicate rescuer fatigue. A rapid increase may indicate ROSC (usually a few minutes before palpable pulse). An EtCO2 value of <10 mmHg after 20 minutes of CPR (in intubated patients) is associated with a poor outcome.
Credit: ERC
"Point-of-Care Ultrasound" (POCUS)
The indication for the use of ultrasound is weakened because of concern that this approach leads to prolonged/multiple pauses, resulting in a worse outcome. POCUS is recommended "only" for experts to search for reversible causes of cardiac arrest. Ultrasound should not be used routinely for prognosis/resuscitation interruption (as the evidence is not robust). Editor’s comment: Emergency teams should therefore be trained in advance in the use of POCUS, the use of which is in any case limited.
Caution in interpretation of dilated right ventricle is recommended. Right ventricular dilation occurs rapidly in the context of circulatory arrest and is often seen even without pulmonary embolism. Editor’s comment: A quick look at the femoral veins may be useful. If signs of thrombosis are evident at this level, a pulmonary embolism can be assumed.
Extracorporeal cardiopulmonary resuscitation (ECPR) / extracorporeal life support (ECLS)
Consider ECPR in specific and selected resuscitation cases to perform therapeutic interventions (e.g. Percutaneous coronary intervention /PCI in myocardial infarction, thrombectomy in massive pulmonary embolism, rewarming in hypothermia).
Termination of Resuscitation / Cessation of CPR
No precise universal guidance is given for ending resuscitation. It is delegated to local health systems to implement criteria for suspending and terminating CPR for both in-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA), taking into account the specific local legal, organisational and cultural context.
It is clear however, the recommendation to not resuscitate if it is not in accordance with the patient's wishes, if there are definite signs of death or injuries incompatible with life, or if there is danger to rescuers. In addition, cessation of CPR may be considered if asystole persists for more than 20 minutes despite ALS and the absence of a reversible factor, or in the event of an unwitnessed arrest with a non-shockable initial rhythm, severe comorbidities or when quality of life already significantly impaired. It is explicitly stated that the following elements should never be used alone to terminate resuscitation: pupil size/reactivity, duration of CPR, ETCO2, comorbidities, or suicide attempt.
The 2021 ERC Guidelines can be downloaded here: New ERC Guidelines.
An overview of the most important ECR Guidelines 2021 changes is available in this esanum article series:
- The ERC Guidelines 2021 (Part 1/7)
- Main Changes (Part 2/7)
- Adult Advanced Life Support (ALS) (Part 3/7)
- Peri-Arrest Arrhythmias (Part 4/7)
- Cardiac Arrest in Special Circumstances (Part 5/7)
- Post-Resuscitation Care (Part 6/7)
- Resuscitation in Children (Part 7/7)
Sources:
1. Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, Lott C, Olasveengen T, Paal P, Pellis T, Perkins GD, Sandroni C, Nolan JP. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation. 2021 Apr;161:115-151. doi: 10.1016/j.resuscitation.2021.02.010. Epub 2021 Mar 24. PMID: 33773825.
2. Fandler M. Neue Reanimationsleitlinien 2021 (ERC) Zusammenfassung. Notfallmedizin.de. 25/03/2021